

(Dave Berg’s theory that ME/CFS patients were in a state of hypercoagulation or thickened blood which reduced oxygen and nutrient flow to their tissues appeared around 2000. The theory, like so many other theories, (eg. Chia’s enterovirus findings), received little attention from the research community. One small study (n=17) did not find evidence of hypercoagulation and that was it for the theory. Ken Lassesen, however, benefited greatly from hypercoagulation therapy and his research lead him to suspect an intriguing blood-gut-infection combination was present in ME/CFS)
“Overall, our findings suggest that clot formation can be a physiological weapon that helps to fight off pathogenic microbes. Indeed, activation of the blood coagulation process is probably an important and widespread antimicrobial defence mechanism.” Englemann
You know B and T-cells go ballistic when confronted with an infection. You may know that natural killer cells poke holes in infected cells or that monocytes into killing machines called macrophages when they ‘hear’ a pathogen is around, but you probably don’t know that immune cells called neutrophils actually thicken our blood to fight pathogens as well.
A clotting factor; recent research suggests the body produces clots to trap pathogens in the small blood vessels
It turns out that upon encountering a microbe the innate immune system initiates an ‘unspecific inflammatory response’ which includes producing small blood clots that trap pathogens in the small blood vessels. (What an interesting finding that is given Dr. DeMeirleirs assertion that the small blood vessels are already clamped down.. )
The Dave Berg/Hemex model for CFS and GWI involves an infection causing excessive coagulation due to a genetic or an acquired (often from organphosphates) coagulation defect. A coagulation defect occurs when a glitch in the complex coagulation process that allows coagulation products to remain and build up over time.
To give an analogy, coagulation is more complex then burning fossil fuels. When we burn such fuels, carbon monoxide, carbon dioxide, water, sulphur dioxide (“bad eggs smell”), even arsenic are released into the air and local environment. Nature re-absorbs most of these chemicals — but if the right circumstances happen, one or more may start to accumulate and may cause a local health issue — it may be just smog or can even be toxic ground water.
The same is true for coagulation disorders, even more so.
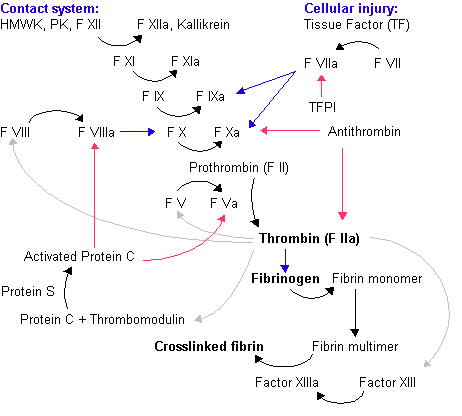
Coagulation cascade
A coagulation defect means that one or more of the above arrows are missing or not working. For myself, it’s the links between Prothrombin(F II) –> Thrombin (F IIa) –> Fibrinogen –> Fibrin monomer. Correcting this particular defect required nothing more than adding turmeric and piracetam. Another ME/CFS sufferer had problems with the Protein S link. This style of defect is rarely clinically significant (i.e. not worth exploring by MDs) unless there was something causing coagulation to keep the process going and going at a higher level than normal. If a stroke occurs, then MDs will take action.
That something could be an infection or a toxin.
Dave Berg discovered this CFS connection because his lab specialized in testing for coagulation issues associated with infertility. (Accumulated coagulation products can interfer with the flow of oxygen to the fetus can cause an abortion.) The treatment for this type of infertility is low doses of the body’s natural anticoagulant compound – heparin.
Similar to what happened with Rituximab 10 years later, the MD’s of these infertility patients noticed that many of their ME/CFS patients got better when on heparin. Many of these patients had thick enough blood to receive a diagnosis of anti-phospholipid syndrome (APS) or Hughes Syndrome. Berg’s investigations lead to several publications before he retired.
- Berg D, Berg LH, Couvaras J, Harrison H. Chronic fatigue syndrome and/or fibromyalgia as a variation of antiphospholipid antibody syndrome: an explanatory model and approach to laboratory diagnosis. Blood Coagul Fibrinolysis. 1999 Oct;10(7):435-8.
- Harrison H, et al. Procoagulant genetic factor in a pooled cohort of 582 chronic fatigue syndrome, fibromyalgia and related chronic illnesses, AACFS, Oct 2004
- Hannan KL, Berg E, et al. Activation of the coagulation system in Gulf War Illness: a potential pathophysiologic link with chronic fatigue syndrome: a laboratory approach to diagnosis. Blood Coag Fibrinolysis 2000, 11:7
For more on anti-phospholipid syndrome, ME/CFS and David Berg, check out “Conversations with David Berg” here.
So that’s the back story for this post…
Microbiome or Infection or Both?
Last time around, I was working off an infection causing model. In my readings, I found that the infections associated with a condition called Hughes Syndrome a.k.a. antiphospholipid antibody syndrome appear to be the same ones that are over-represented in the CFS population. My primary sources for APS infections was From “Hughes Syndrome Antiphospholipid Syndrome” Springer, 2000 (2nd printing 2002), editor M.A. Khamashta. Chapter 14, “Infections and Antiphospholipid Syndrome”(by A.E. Gharavi and S.S. Pierangeli), p. 135.
| Chronic Fatigue Syndrome Associated Infections | APS Infections |
|---|---|
| EBV (20% – 72%) — 11 articles on pubmed | Epstein-Bar Virus (EBV or HHV4) |
| VZV – 2 articles on pub med |
Varicella zoster virus (VZV or HHV3 -chicken pox) |
| ** | Human Immunodeficiency virus (HIV) |
| HHV6 (25% – 58%) – 12 articles on pub med |
Human Herpes Virus 6 (HHV6) |
| CMV (29%) – 4 articles on pub med |
Cytomegalovirus (CMV) (HHV5) |
| Coxiella Burnetii (Rickettsia)(90% – 50%) – 6 articles on pub med |
Coxiella Burnetii (Enteroviruses) |
| Lyme – 2 articles on pub med |
Lyme Disease (Rickettsia) |
| Mediterranean spotted fever (Rickettsia) | |
| Mycoplasma (41% – 69%) – 13 articles on pub med |
Mycoplasma |
| Anecdotal – see below |
Leprosy |
| ** | Tuberculosis |
| ** | Syphilis |
| Parvovirus B Three articles on pub med |
Parvovirus B |
| ** | Hepatitis |
| Chlamydia-Pneumonia (8%) – 4 articles on pub med |
Chlamydia-Pneumonia – 3 articles on pub med |
| Human Enteroviruses (32% – 82%) 2 articles on pub med |
The bottom line is simple: infections known to cause APS tend to be over represented in ME/CFS patients. Most of the infections associated with ME/CFS are known to cause APS (with one exception)
The anecdotal case of leprosy is interesting because I met someone at a Seattle ME/CFS Support group meeting who had and was successfully treated for Leprosy but came down with ME/CFS afterwards. Retesting her for leprosy indicated she was all clear. My assumption at that time was that a co-infection was responsible…. In 2012, however, a mathematical modelling article changed my opinion totally….
This article, which ironically, dealt with the same type of machine learning I was doing at Amazon before my relapse, proposed that an analysis of a person’s gut microbiome could provide greater than 90% accuracy in determining what infection/illness. It suggested that each of the above infections alters the gut microbiome for its own benefit and that the symptoms caused by the infection could, in some cases, be due to the altered microbiome – not the infection, per se. This article suggested that sometime in the future, your family MD may ask you to bring in a stool sample in order to figure out what’s wrong the matter with you!
Then another mathematical modelling study, found that the longer that a person has an infection, the more likely that the microbiome will stay in its altered state. That is, the microbiome associated with the infection will persist (and thus accounts for the ease of re-infection for some diseases). This altered / unhealthy microbiome will keep pumping out signal chemicals causing coagulation and other symptoms without the infection being present.
You may test negative for every one of the infections above and still have the symptoms!
This ‘hit and run’ theory in which a pathogen hits, does its damage by altering the homeostasis of an organism, and then disappears, is a prevalent one in ME/CFS given how difficult the Dubbo studies indicated it was to find active virus/bacterial infections in people with infectious onset. That suggested to me that the search of an infection causing CFS may be an ideological quest doom to failure. It might be far better to look for evidence of chronic system dysregulation, and, for me, that system was the gut.
Ten years later, doctors are not ordering stool samples in order to find out what infection you have but based on my experience and my readings, I believe that an altered microbiome alone could account for many symptoms of chronic fatigue syndrome. I am not saying that checking for the above infections should not be done — definitely they should (and if found treated), but that may be only part of the CFS engine. The other parts need to be addressed also.
In the next posts I will look at what what we know about the microbiome (not that much) and how to alter it (even less)…







The blood, the brain, the muscles, the tissue, has been examined for years, looking for the cause of CFS! No success.
We don’t know much about the region, where the immune system resides, (in the gut), so, no reason to focus there.
I suppose, mucking around in the microbes in the gut isn’t romantic, or, very appealing but it is the “last frontier” of the medical world. If there is dysbiosis in the gut, is it so surprising, the immune system would suffer??? RP
I tend to be a strong lateral thinker. One side effect is that for every reaction, you can see that it may be caused by 5, 10 or a hundred different actions may be it’s cause. Many people, especially MDs, tend to vertical thinking – often as a survival technique to information overload.
In dealing with CFS and other autoimmune disease, it is best never to ask “Is it A or B?” Instead, “Is it A, Or B, Or A interacting with B, Or some other factor C interacting with A and B?”
For THE infection causing CFS, the latter question became “Is it due to one of this collection of infections that also causes APS?” There is no longer a ONE infection question, rather a family of infections that are all know to trigger low level coagulation.
When it comes to symptoms – it similarly becomes: Is it the infection causing the symptom OR/AND is it the body response to the infection … which I recently added, OR/AND the changes to the body’s microbiome sparked by the infection.
My theory does have one major defect, it is far more complex than the usual disease model. Using the model results in treatment complexities that must be done by “feel” and not by explicit testing following by the appropriate application of some prescription drug.
“We hypothesize that damage or stimulation of the mitochondria results in the release of phospholipids, which in turn induce production of an autoimmune antibody (antiphospholipids).” from
Acute Phase Phospholipids Related to the Cardiolipin of Mitochondria in the Sera of Patients With Chronic Fatigue
Syndrome (CFS), Chronic Ciguatera Fish Poisoning (CCFP), and Other Diseases Attributed to Chemicals, Gulf War, and Marine Toxins
http://www.ncbi.nlm.nih.gov/pubmed/18348309
Note the “hypthesize”, there are several articles on pubmed dealing with phospholipids and microbiome/ gut bacteria where results were actually demonstrated. A few examples are:
“The gut microbiota has recently been identified as an environmental factor that may promote metabolic diseases. To investigate the effect of gut microbiota on host energy and lipid metabolism, we compared the serum metabolome and the lipidomes of serum, adipose tissue, and liver of conventionally raised (CONV-R) and germ-free mice. …We also showed that the microbiota modified a number of lipid species in the serum, adipose tissue, and liver, with its greatest effect on triglyceride and phosphatidylcholine species.” http://www.ncbi.nlm.nih.gov/pubmed/20040631
” Daily intake of dark chocolate significantly increased HDL cholesterol by 6% and decreased polyunsaturated acyl ether phospholipids..” http://www.ncbi.nlm.nih.gov/pubmed/23163751
Which may account for why 10% of the participants of a study testing 200gm of 85% chocolate daily were able to return to work… Trade Joe has a suitable bar at $1.49 for ~ 200 gm…
Hi Ken I am very interested in what you are saying about gut bacteria. I was wondering if you feel that a quicker more effective and permanent way to fix the gut dysbiosis is with the use of antibiotics or do you think it is better to just keep adding the correct strains? I have a entero, staphylo, strepto, kliebsiella and Bifido overgrowth while being low in bactericides, lacto, clostridium and e.coli. I have previously felt some improvement from big amounts of yogurt but it did not last. I am going to try prescript assist and mutator but am wondering if you think I would be best lowering the numbers of the overgrown bacteria first? Can prescript assist be cultured? Do you know of the strains that are responsible for the production of the neurotransmitter a like serotonin and dopamine? I know there is a lot of interest in this at the moment. I have also come across a few products containing strains you haven’t mentioned if you are interested. Thanks for your help.
I wish that I could give a definitive answer but there is no objective evidence to answer from. I believe that the tetracyclines (minocycline, doxcycline, etc.) are the most probable antibiotics to be of help. This belief is due to the significant success of Jadin, Nicolson, etc. For probiotics, E.Coli and L.Reuteri are likely the key ones that are obtainable. L.Reuteri is typically 50% of the Lactobacillus in most mammals. The other lactobacillus species in probiotics are likely “flow-thru” only.
To lower overgrowth, my preference (based only on a very limited case reports) are Neem, Tulsi and Haritaki. Why? Some studies found that they are as effective as some of the more powerful antibiotics, they do not require prescriptions, 500gm / 1 lb is just $20 (which gives you a year of pills), and they seem to impact neurological issues.
What we did was the two week ramp-up, one “00” capsule on day 1, and keep adding more every 24 hours until you are feeling a significant impact… keep that dosage until the 7th-10th day and then go off for 2-3 weeks. Pulsing with rotation. One week may be haritaki, next week Tulsi, then Neem, then other items like wormwood or olive leaf could be tried. By rotating, you reduce the risk of resistance happening. There is a PubMed study from China where E.Coli developed resistance to various herbs when they were continuously being taken.
Please tell me the name of the strains [hoping that they are not Lactobacillus]…
Ken, where do you get the herbs in bulk that you mentioned in your article?
Thanks for the info and please keep it coming as far as your own personal experience with these probiotics and herbs.
I found Dr. Natasha Campbell McBride whom you mentioned regarding the Perscript-Assist at another web site that you did not mention. It is wwwgutandpsychologysyndrome.com At that site she offers probiotics in capsule and powder form but with a different name and I’m wondering if it is the same probiotic you call Prescrip-Assist or is it something different?
You can buy them off amazon or in some Indian Grocers.
Usually I use Banyan Botanicals ( http://www.banyanbotanicals.com/ ) which have a wide arrange of of Ayurvedic herbal products.
http://www.banyanbotanicals.com/prodinfo.asp?number=7361 Neem, 1 lb, $19
http://www.banyanbotanicals.com/prodinfo.asp?number=6731 Tulsi, 1 lb, $21
http://www.banyanbotanicals.com/prodinfo.asp?number=6901 Haritaki 1 lb $18
http://www.banyanbotanicals.com/prodinfo.asp?number=6751 Turmeric, org (1 lb.) $18
The above is more than 1 year supply of each for… under $80…
The McBride probiotic is NOT the same. Prescript assist has ~30 species, none of them Lactobacillus. Her’s has:
Lactobacillus plantarum
Lactobacillus gasseri
Lactobacillus salivarius
Bifidobacterium bifidum
Bifidobacterium infantis
Bifidobacterium longum
Bifidobacterium breve
Bifidobacterium lactis
So just two familes and many are available in other probiotics.
Ken, where do you get the herbs in bulk that you mentioned in your article?
Thanks for the info and please keep it coming as far as your own personal experience with these probiotics and herbs.
I found Dr. Natasha Campbell McBride whom you mentioned regarding the Perscript-Assist at another web site that you did not mention. It is wwwgutandpsychologysyndrome.com At that site she offers probiotics in capsule and powder form but with a different name and I’m wondering if it is the same probiotic you call Prescrip-Assist or is it something different?
I’m not sure about that GAPS diet since I do not like meat, it tends to make me nauseous. I’m thinking about going low fat vegan for a while to see if my health improves.
I just found this article – so a little late in commenting. But, you’re not alone in what you think with a possible cause of a protozoa or bacteria etc. causing the issues. I’m seeing a doctor who has discovered a protozoa and is doing research that could very possibly be THE main cause of all of our issues —be it CFS, FMS, POTS, OI, ALS, MS etc. Here is an interview that he recently did – explaining his discovery and what he feels it is contributing towards with health issues.
http://protomyxzoa.org/wp-content/uploads/2013/04/Protozoal-Infection-Dr-Frye-Interview.pdf
I have been doing a low fat, vegan diet and addressing a positive test for this protozoa and co-infections related to Lyme with doxycycoline and supporting anti-malarial herbs, along with probiotics and other things that address the immune system. I’m getting very good results with this approach. I’m not well, but making huge improvements. The things used, also thin the blood – and I too find that turmeric is a big help to me. Interesting, the suggestion of pulsing antibiotic type herbals – as this is one thing done to “control” protozoa. They are known to live in a bio-film which incases them and sort of forms a protective shield around them and the immune system can not detect them. You have to break down this biofilm so that the immune system can recognize what is living in it – protozoa, bacteria, virus etc.
I’m really impressed with my results so far. Something worth taking a look into for sure.
Issie
The good result is nice to hear! I’m a scientist by training and a lateral thinker. What I have read over the last 15 years is positive results from doing X because Y is suspect. Because the results are good, physicians slip into believing the Y is correct and the answer.
My approach this relapse (followed by remission) was to keep searching laterally for a model that is consistent with ALL of the positive results reported in the literature and conference reports. The simplest (Osler Principle) was a stable dysfunction microbiome.
With a model that is consistent with the data, the next stage is use the model to discover/predict approaches that is not in the literature and see if they produce additional positive results. So far, the model appears to be holding as valid. If someone can come up with a better model with the same amount of supporting evidence, I am very willing to consider it.
The interesting thing is that the microbiome can alter the chemical circulating so that formerly controlled infections are mildly re-activated. These infection, co-infections, appear to be likely consequences and not the cause, IMHO.
Issie,
I read that link and it was very informative for me. I am going to try a low fat vegan diet and see if that helps me. Going off of magnesium will be a challenge for me since it helps my pain so much. I wish I could do a hot tub or sauna. That idea is intriguing to me that the warm temps can help with the protozoa. Thanks for the info!
I hope it makes a difference for you. With me, I’m seeing very good improvements. Just make sure you keep your plant protein levels up. I use a program called SparkPeople (it’s free) and you can enter what foods you eat and it gives you a nutritional breakdown of how you’ve done for the day. That helps me to be able to make better food choices and make sure I’m keeping my nutrition up. It’s especially important as you are first learning how to eat this way. You will be surprised how hard it is to stay low fat. Vegetables have fat in them too. They also have a place where you can get vegan recipes and start your own cookbook with recipes that you copy. It’s a really good site.
Issie
Issie,
I found the Sparkpeople and signed up.
Now, I will try and educate myself on plant protein. I know some basics like beans and rice. Thanks for the info.
Look at the McDougall diet and also Forks over Knives and Engine 2. Lots of info and recipes there.
Let me know how you do.
Issie
Whic herbs, Issie?
I would suggest looking at http://cfsremission.wordpress.com/treatment/microflora-and-autoimmune-illnesses/changing-microflora-by-herbs-and-spices/
You will find the three most effective according to the literature — and the links to the studies.
Interesting thoughts about the chemical circulating causing the reactivation of the infections. (What’s your hypothesis on that?) My doctor has determined with this protozoa that magnesium and arginine increases the strength of the biofilms and the protozoa love this – as it helps them to avoid detection. He has also found that fat in the diet is what they love and it will help them to multiply. It could be something as simple as our diet that is increasing this “force field” and preventing our immune system from recognizing the things we want it to see and eliminate. How often do we eat something or take even a natural supplement and maybe we are doing damage to ourselves by keeping something alive and active that we’d rather be rid of. Could we be creating our own sickness by our ignorance? Ultimately, my thoughts are that first we are genetically predisposed to things and then there is a faulty immune system and along with that for a close second is inflammation. Work on those things and see where we get. If we can determine faulty genetics that we maybe can correct with nutrition and that will work on the immune system which in turn should help with inflammation. That’s the direction I’ve gone with working on myself. So far, that approach is proving to be beneficial.
I love looking at things from different angles. If you only have one view of the picture, you won’t get the whole picture. If what is the commonly accepted view is found to not be complete, we have to continue to look for alternative answers. So far, the picture is not complete. I like the terminology of “lateral thinker” – beats the term “out of the box thinker” – which I consider myself being. Keep up your “lateral thinking” and keep putting it out there. Who knows what us that think this way may come up with.
Issie
I do not think that we are predisposed in the usual sense. There is inheritance of gut flora, which agrees with CFS running in families. Diet impacts the growth of species. I just heard a broadcast that compared diet in 1946 to today. The amount of green vegetables per week had decreased by 80% and the amount of wheat (buns, breads, etc) has increased more than 4x.
I do not believe it is in our DNA genetics, but is in our microbiota genetics.
Yes, I think diet plays a big role in a good bit of the dysfunction that we see today. A change of diet will change the gut flora – either in a good direction or a bad one.
I’ve had genetic testing done through 23&me and found that I’ve got the genes for some pretty bad illnesses. But, I have not developed those illnesses. I’m hoping that I can keep them from manifesting with what I do for my body. If I can keep things in balance and not activate something that I don’t want —-I’ll be extremely Happy.
Issie
If you look at the AmericanGut project, specifically this PDF, http://americangut.org/wordpress/wp-content/uploads/2013/09/module1_Sept_16_small.pdf you will see that what is in the gut varies greatly from country to country.
I once worked with a group of WW2 veterans and they mentioned that they could tell what nationality that the dead was by their smell alone. Because of the different gut bacteria that went with each diet, there was different chemicals being given off by each corpse.
Ken,
When I was tested years ago, I had a very high Thrombin-Antithrombin Complex value. Does that have to do with coagulation?
Yes, it does deal with coagulation, this “TAT” can be a sensitive parameter for detection of a latent activation of the clotting pathway. This typically indicates some disease process is happening (http://www.karger.com/Article/Pdf/227620 for an example). Which disease cannot be determined – it may be bacterial, viral, etc.