



“There is a huge overlap between these different syndromes” Dr. Peter Rowe
If you watch this video you might want to skip over Dr. Henderson’s remarks if you’re a little sensitive, as I am, about ME/CFS’s place in the research world.
Henderson started off by stating that Dr. Rowe was the first man to highlight the interrelationships between orthostatic intolerance (OI), fibromyalgia and Ehlers-Danlos syndrome and notes that Dr. Rowe runs the fibromyalgia clinic at Johns Hopkins.
.Actually, Dr. Rowe does not run the fibromyalgia clinic at Johns Hopkins; he runs the Children’s Center Chronic Fatigue Clinic. He has not elucidated the relationships between FM, Ehlers-Danlos syndrome, and OI; he’s highlighted the interrelationships between ME/CFS, ED, and OI. In fact, he’s published many more papers on ME/CFS (13 papers) than on either ED (2) or fibromyalgia (1). If Dr. Rowe is anything, he’s an ME/CFS guy. In fact, Rowe will refer to chronic fatigue syndrome, not fibromyalgia, throughout the talk.
OK, my rant is over. Henderson was absolutely right, though, about the ‘unity’ being uncovered between all these ‘tightly interrelated’ disorders. That’s a fascinating aspect of ME/CFS/FM/ED/POTS, etc., that we’ll be exploring more in the future. He’s also right that Rowe has been and continues to be a pioneer in these fields as he continues to open new ground.
How Rowe got to Chronic Fatigue Syndrome
“The chronic fatigue syndrome patients really were very much like the fainters”

Despite fainting less than the ‘fainters’ , people with chronic fatigue syndrome had far more circulatory issues
Rowe got to ME/CFS in much the same way Dr. Newton in the U.K. did. Both were interested in fainting (Rowe in OI, Newton in the elderly) and gradually got introduced to a group of patients that nobody knew what to do with–the ME/CFS group–and found, to their surprise, that they were much like the ‘fainters’ even though they didn’t faint as much.
Both the fainters and the ME/CFS patients got into trouble by standing, shopping, or being in a hot environment, and both responded significantly to a tilt table test. To Dr. Rowe’s astonishment, the ME/CFS patients fared much worse than the fainters on the tilt table test.
“What we recognized very quickly was that the chronic fatigue patients, who many in the medical community felt were just a bunch of whiners and complainers trying to get out of the stress of life, had much more profound circulatory problems than the people who were fainting.”
That first paper he published to that effect, Dr. Rowe said with a smile, changed his life, because the 5,000 phone calls he got made him realize “there might be a tiny unmet need out there.”
Case Study
All good talks by MDs have at least one good case study, and Rowe had several. In the first an adolescent girl, just 12 years old, comes down with mono, seems to mostly recover, but then starts sliding. By age 15 she’s getting wiped out by things like shopping, playing in the band, standing in showers, and choir practice. She experienced light-headedness, had unrefreshing sleep, joint pain, post-exertional malaise, and was going downhill cognitively. In addition,
Rowe notes in passing that in infancy she couldn’t ‘handle milk’ (where ‘not handling it’ meant she would scream every time she was given milk products.) But her milk sensitivity seemed to resolve by age two, and was now showing up again. (Twenty-five percent of Rowe’s cohort has milk intolerance. Since milk intolerance can cause all sorts of symptoms, Rowe finds it necessary to get milk intolerant patients off of milk in order to tell how effective his treatments are. He now looks carefully for milk intolerance in all his patients.)
Over time this young woman developed no less than three syndromes. the last Chiari malformation, apparently brought on by a cold
Welcome to Chronic Fatigue Syndrome (ME/CFS)
In his office, Rowe sees a ‘very poised’ young woman, diagnoses her with ME/CFS and then it gets really interesting.
First, he noticed her ‘velvety soft skin’ that was ‘very stretchy’ in some areas, her ‘very stretchy’ upper eyelids, her ‘high palate’, pressure bumps on her feet when she stood, and blue in the whites her eyes. Finally her Beighton hypermobile score was 8/9 where 4/9 signals possible hypermobility.
Welcome to Ehlers-Danlos Syndrome (EDS)
Standing her up against a wall for five minute caused her heart rate to more than double, from about 50 bpm to about 110 bpm.
Welcome to Postural Orthostatic Tachycardia Syndrome (POTS)
Treatment – Florinef, midodrine, lots of salt and increased fluid intake and she was on her way… until back to back colds (nothing special, Dr. Rowe said) left her very fatigued, unable to sleep, and with severe headaches. She dropped out of school. Somehow, in the midst of her improved health two small colds had wiped her out.
A visit to the Clinic revealed a different young woman; now she couldn’t follow the doctors finger as he waved it back and forth (nystagmus), her gag reflex was mostly gone, and he had hyperactive reflexes elsewhere. An MRI revealed her brainstem is bent forward and a bone is pressing against it, her tonsils have dropped, and her brain is engorged with spinal fluid because of the obstructions now present around her brainstem.
Two surgeries later, she was doing better. Dr. Rowe did not go into how an infection caused these anatomical abnormalities.
Basics
Rowe next laid out some disease basics.
Orthostatic Intolerance refers to being unable to stand without symptoms, usually because not enough blood is getting to the brain. Half of the symptoms associated are orthostatic intolerance (dizziness, fainting, poor concentration, headache, blurred vision, exercise intolerance–if you thought PEM was exclusive to ME/CFS, think again) are due to the loss of blood to the brain.
The other symptoms (shortness of breath, chest tightness, palpitation, shakiness, anxiety, and nausea), it is interesting to note, are the result of the body desperately pumping out adrenaline (epinephrine) to get blood back up to the brain.
Orthostatic Intolerance (OI)
Rowe mostly sees two kind of OI.
Neurally Mediated Hypotension (NMH)
NMH signifies a drop in blood pressure that sometimes occurs very rapidly. Dr. Rowe pointed to a graph showing one person doing just fine for the first four minutes only to have her blood pressure (and heart rate) abruptly plummet in the fifth minute. As her blood pressure hit zero, she began having seizure-like symptoms. As soon as she hit the floor, though, her blood pressure went back up to normal.
Postural Orthostatic Tachycardia Syndrome (POTS)
POTS is defined by a 30 beat per minute (bpm) increase in heart rate during the first ten minutes of standing in adults, and a 40 bpm increase in adolescents, or a heart rate above 120 bpm. The heart rate increase must also be accompanied by relevant symptoms.
There are healthy people with POTS. As we’ll see with Ehlers-Danlos Syndrome, some people who meet the POTS criteria are as healthy as can be.
Other features
Dependent ‘acrocyanosis‘ is a purple mottled color in the hands and legs when standing. Rowe showed a dramatic picture of three white splotches on a patient’s legs where he had pressed his fingers and then had stood back and taken a picture. That kind of finding in an intensive care unit would have them “all over you,” he said.
There are two main problems going on in OI: one is low blood volume, and the other is trouble constricting the blood vessels in their legs upon standing.
POTS can be traced back at least to the Civil War where it tended to show up after battle and was referred to as irritable heart, effort syndrome, battle fatigue, and later neuro-circulatory or “nervous system exhaustion” (bringing to mind the ‘neurasthenia’ ME/CFS was probably diagnosed as back then.)
That Gender Imbalance Again – As in ME/CFS, FM, and Sjogren’s Syndrome, probably about four times as many females as males get POTS and, as in ME/CFS/FM, etc., a variety of stressors can trigger it, including mononucleosis (a major trigger in ME/CFS), trauma, surgery, etc., or it can have a gradual onset.
Other Complications – Dr. Rowe warned that many doctors who focus on POTS miss the other autonomic symptoms present such as night sweats, gut issues, temperature regulation, and then presented a quote that Lauren Stiles, a POTS patient who didn’t rest until she got answers, surely agrees with. Her experiences suggest the quote below should be on every POTS specialist’s wall.
“We should view the POTS diagnosis as a starting place for the discovery of the cause of the patient’s problems rather than a final answer as to what the patient actually has.”
A Treatment Protocol That Works (If You Can Get To It)
In an early study Rowe found that ME/CFS patients with orthostatic intolerance came in at about 35 on a 1-100 Wellness Scale, and after 4 months on average most were up to the 60-70 range, which is a huge jump.
Dr. Rowe’s basic treatment plan includes:
- Increase blood volume: drink 2 liters of liquid a day, increase salt intake, florinef, birth control pills, clonidine.
- Increase vasoconstriction: midodrine, dexedrine, methylphenidate, SSRIs, SNRIs, aescin (horse chestnut seed extract).
- Decrease the effects of epinephrine/norepinephrine release: beta blockers, disopyramide, SSRIs, ACE inhibitors.
- Misc: pyridostigmine bromide, droxidopa.
- Checking for allergies, particularly milk allergies.
In this quickie overview Rowe does not mention immunomodulators such as IVIG (which helped Lauren Stiles greatly) or autoimmune drugs such as Rituximab (Rituxan) which might be able to help POTS patients with autoimmune disorders. Lauren Stiles’s course of IVIG is an unusual treatment in both POTS and Sjogren’s Syndrome, both of which she has, but her success with it suggests it may be useful in more POTS/ME/CFS/FM patients.
In early results Dr. Teitelbaum is having success with IVIG in some of his most difficult to treat patients with small fiber neuropathy, and Dr. Sivieri’s findings of low IgG subclasses in his FM/ME/CFS patients has prompted him to use IVIG there. Since both of these disorders have substantial overlaps with both POTS and ME/CFS, it’ll be interesting to see how effective these doctors find these drugs over the next 6 months to a year.
Rowe’s Next Big Step
Rowe’s view of these disorders is continually evolving. Rowe’s discovery of an intriguing neuromuscular component to them is not covered in this talk (we’ll get to that later) but the next step demonstrates how an inquisitive doctor/researcher learns. Rowe sends a patient with B-12 problems to an Irish geneticist with a hearty sense of humor who came back to him saying (in a nice Irish brogue), “Peter, do you ever actually examine your patients?”
It turns out this person has a big Ehlers-Danlos Syndrome scar on her leg; that finding prompts Rowe to start looking for EDS in other patients, where he finds it in surprisingly high quantities. The texts say EDS occurs in about one in every 5,000 people, but Rowe finds it in about 10% of his ME/CFS patients. All of them also had orthostatic intolerance.
Ehlers-Danlos Syndrome
Several different forms of this connective tissue disorder (e.g., skin, joints, muscles, blood vessels) exist, but some of the key characteristics of the kind of EDS found in ME/CFS/FM are:
- Hyperextensible , very stretchy skin
- Hypermobile, hyperflexible joints
- Fragile skin–easily bruised, easily torn
- Early onset varicose veins
- High fatigueability
- Widespread pain
About Ehlers Danlos Syndrome
Beighton Score For Hypermobility
You can score your degree of hypermobility using the Beighton questionnaire
1. Extend the first finger (2nd digit) over the back of the hand—if 90 degrees or greater score:
- 1 point left
- 1 point right
2. Flex the thumb toward the forearm—if the thumb touches the forearm
- 1 point left
- 1 point right
3. Extend the arm—if 10 degrees or more of hyperextension at the elbow
- 1 point left
- 1 point right
4. If 10 degrees or more of hyperextension at the knee
- 1 point left
- 1 point right
5. Flex at the waist—if you are able to touch your palms to the floor score:
- 1 point
Total your points and compare below:
- 1-3 points—low flexibility
- 4-6 points—moderate flexibility
- 7-9 points—high flexibility
Young Woman Demonstrates Ehlers Danlos Syndrome
As with POTS, EDS is about more than hypermobility. The fact that healthy people can be hypermobile suggests the disorder is more than about loose connective tissue. One study showed that 20% of healthy people meet the Beighton criteria for hypermobility, and Dr. Rowe showed a picture of a grandmother with hypermobility who was healthy but whose kids were hypermobile, orthostatically challenged, and sick. Hypermobility, then, is a risk factor for ME/CFS–not a determining factor.
- Dig Deeper – Ehlers Danlos National Foundation
Cause
The big question, of course, is what is causing Ehlers-Danlos Syndrome, POTS and orthostatic intolerance to show up together? Why should hypermobility lead to difficulty standing? Several theories exist.
- Rowe believes connective tissue laxity causes the blood vessels in the legs to bulge and allow blood to pool in them upon standing.
- Benarroch believes joint dislocations and pain hypersensitivity (somatosensory amplification) plus anxiety lead to physical inactivity and hyper-sympathetic responses triggered by fear of pain upon standing. Rowe does not subscribe to this.
- Peripheral neuropathy: we’ve seen Lauren Stiles story where an autoimmune disorder wiped out many of her autonomic nerves causing both blood pooling in her legs as well as POTS.
- Excessive mobility of the spinal cord at the neck causes autonomic nerve compression, fatigue, problems standing, digesting issues, etc.
With that we head over to the spinal cord and some fascinating case histories.
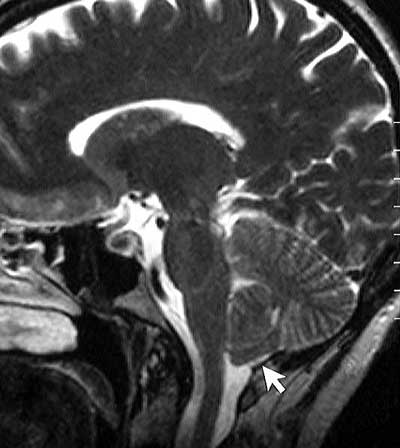
A Chiari malformation that blocks the flow of spinal fluid back into the body can cause headaches, fatigue, muscle weakness, problems swallowing, nausea, etc.
Narrowed Cervical Canal Whacks Autonomic Nervous System Functioning
Dr. Rowe described one young woman with a narrowed cervical canal. After a disc decompression to fix a vertebrae impinging on her spinal cord, this young woman – who’d been unable to attend school – garnered a job walking dogs at a month and half later, and at six months (almost tempting fate, one might think) she’d become a horse-wrangler. She is now back in school full-time.
Chiari Malformation Plus
An active 15-year-old first experienced headaches, then numbness and tingling, and finally her continuous headache (migraine) knocked her out of school and eventually into Dr. Rowe’s office. She too had nystagmus (couldn’t track right to left with her eyes), and a positive Romberg test. Her MRI showed a Chiari Malformation. After ‘decompression’ her headache disappeared, but then it later came back.
Rowe then examined her again and found several symptoms indicating orthostatic intolerance (had visual blackouts, had trouble with heat, felt mentally dull). At two minutes on the tilt table test her headache came back, at eight minutes she felt hot–a clear indication of an adrenaline (epinephrine) surge and often a prelude to, as Dr. Rowe called it, a ‘face-plant’. Sure enough, her blood pressure was dropping dramatically and she had to sit down.
With salt tablets, midrodrine, florinef, and pindolol she was back in school, and is now a senior in college, with a 4.0 GPA, and is applying for medical school.
About Chiari Malformation
Chiari Malformation Take Two
Chiari malformation usually refers to ‘dropped tonsils’ which obstruct the passage of spinal fluid out of the brain causing the spinal fluid to back up, and resulting in fun things like headaches, fatigue, muscle weakness in the head and face, difficulty swallowing, dizziness, nausea, impaired coordination, and even paralysis.
Another patient with Chiari malformation who failed to respond to a Chiari repair had a cervical fusion to reduce his cervical hyper-reflexibility which was causing his spinal fluid to back up every time he bent his head forward. In his case he had two spinal issues: chiari malformation and a hyperflexible neck.
Rowe noted that the surgical approach still has a lot of grey area; some people respond very well and others do not, and they’re not sure why.
Question Period
Asked who is your counterpart in the adult world at Johns Hopkins (Rowe only sees young people) Rowe noted there was none. He noted that he’s inundated with requests for consultations, at one point last summer getting fifty a week. He has enough work to keep five physicians and nurse practitioners busy but his hospital, which is under financial constraints, is not interested in expanding his clinic.
Another Subset
The subsets just keep coming. Eosinophilic esophagitis is a miserable condition associated with pain, nausea, and vomiting in children. It appears to be showing up in this EDS/OI cohort as well.
Eosinophilic esophagitis is an inflammatory condition in which the wall of the esophagus becomes filled with large numbers of eosinophils, a type of white blood cell. It’s associated with allergy.
The major symptom in adults with eosinophilic esophagitis is difficulty in swallowing solid food (dysphagia). Specifically, the food gets stuck in the esophagus after it is swallowed. Less common symptoms include heartburn and chest pain. In children, the most common symptoms are abdominal pain, nausea, vomiting , coughing, and failure to thrive.
Finding that prednisone for asthmatics helped some children’s gut symptoms, one doctor put them on a (chopped up) amino acid diet and their symptoms dropped dramatically. The response was dramatic enough that the practitioner joked that some parents were writing him into their will. J
Conclusions
This story underscores the need to see an experienced practitioner who’s up on the possible causes of POTS, EDS and ME/CFS. Probably few ME/CFS experts check, for instance, on for a Chiari Malformation or vertebrae impingement in their patients.
That kind of neuro-anatomic issue has mostly been associated with fibromyalgia, but the overlaps between all these conditions are substantial; what condition you get diagnosed with may very well depend on which practitioner you see. It makes sense that ME/CFS practitioners know all the ‘FM’ therapies, the POTS therapies, how to diagnose EDS, etc. and vice versa. (Nobody ever said this field was easy :))
The upside is that a range of treatments are available that in the right hands do work. Rowe’s early study showed he was able to significantly help many people with these conditions. The key for the patient, then, is getting diagnosed and getting to the right practitioner. We’ll have more on that process in future blogs.













I enjoyed this video and seeing that there are so many connections with all these things. I’ve often said if they find the cure for one – the others won’t be too far behind. At the very least, maybe we will know the cause of the problems.
There were some things suggested as meds for POTS that some of us question and wonder if long term effects may make us worse. But, it was a good presentation as to the different things that could be playing into this.
I appreciate that you brought in all the other components of things that are known to cause/contribute to the dysfunction associated with POTS and/or CFS. There have been some of us – especially those of us with EDS, that have found Chiari problems (cerebral tonsil drop). But, few doctors will treat it and as this video shows the surgery is not always a success. Some of us have very unstable necks/spines and the Dr. Henderson that is on this video briefly – does a lot of surgeries to fuse vertebrae in those of us with EDS to help with this and some find it helps them.
There is also talk about CCVSI – which was not talked about here and problems with blood flow through the neck veins and some are trying stents to open these veins up and help with that. Then there is hydrocephalus or inability of spinal fluid in the brain to drain properly. Some are having stents for this too. There are mixed reviews as to the benefits of these stents in either case.
Then we have EDS and lots of problems that goes along with that in regard to blood flow, vein contractions and stability.
So many of us are finding autoimmune connections.
MCAS problems also give many problems similar to POTS. Sometimes, it’s hard to tell when one is having a “potsie day” or it’s a mast cell degranulation.
Thankfully, we have some docs really trying to get to the “core” problem and many of us are trying to get the word out about the connections we’ve found in ourselves and trying to get others to notice if this could be a part of their puzzle too. The more connections we can make – instead of everything being so fragmented – the more chance we will have of finding solutions.
Cort, I know some of this you are just learning about —but, you did a good job in your summary.
As Dr. Rowe indicated, the doctors really looking into all this are FEW and far between. We pretty much have to educate our doctors, unless we are one of the fortunate ones to get to see the specialist. There are lots of tools that are being produced in order to do that. DINET has a brochure and DVD that is available for doctors and they are trying to get names of doctors that may be interested in learning more about Dysautonomia so that we can hopefully help people get the proper DX and not be mis-diagnosed. You can visit the DINET site and send doctors info to them and they will mail out the info to the doctor.
Thanks again Cort – for trying to make others aware of all these complicated puzzle pieces that goes along with Dysautonomia and/or CFS. The questions are many and we need more answers.
Issie
Thanks Issie, I thought the story of the young woman who with POTS who improved but then after two colds had new neurological problems, and then an MRI indicated she had Chiari malformation was particularly interesting. If that malformation was indeed triggered by her cold some sore of immune process in her brain was involved…An infectious triggered anatomical change is amazing.
These are truly complex problems and there’s much to learn. 🙂
I don’t think that the cold triggered the malformation of her cerebral tonsils (brain drop). It just may be that they found this drop when trying to sort out why her POTS was back. Stress, surgeries, pregnancies, illness all have been found to trigger POTS. For some reason, something sets it off. Something flips the switch. If she had POTS before and then went into a sort of remission from her symptoms —something with the virus sent her back into it. (My personal belief is that there probably is a genetic component that gets triggered to turn on. Then there becomes issues with the immune system and inflammation.)
I have a slight drop – what they consider Chiari 0. It’s not enough for them to think it’s causing a problem. But, it also wasn’t measured with upright posture. Us with EDS and over stretchy – could have all sorts of anatomical changes with upright posture – and that could contribute to POTS symptoms – since POTS – supposedly is upright posture related. (Those that have issues with sitting and lying – are finding that MCAS may be playing a part in this. But, I question whether POTS is truly an effect of gravity with upright posture. Since our autonomic system is malfunctioning and that affects every organ and system of our body — POTS is way more than an issue with blood pressures, heart rate and blood flow. We know of other issues related NO levels, NET issues, high angiotension II levels, low renin and aldosterone levels, low blood volume.) It’s just we have more problems with blood flow and fainting with upright posture. Our body tries to compensate more so when we are upright. Even fainting may be a compensation to get us back down to help improve blood flow to the brain and heart. The tachycardia that we get is our bodies way of trying to improve our blood flow. High NE may be our bodies way of trying to constrict blood vessels to help with blood flow. So, why all these issue with blood flow? What is it causing the issues with this? We still aren’t to the core problem. The symptoms are only being treated. Is that the best we can do, just manage the symptoms? Or, can we figure out the WHY of it all and fix the “core” problem and then we won’t have symptoms that have to be masked (masking symptoms may be the wrong thing to do – if it’s a compensation) as an after affect.
Yes, you’re right – there are still many questions left unanswered.
Issie
Given that two surgeries have helped her but don’t appear to have resolved her symptoms you may be right.
“So, why all these issue with blood flow? What is it causing the issues with this? We still aren’t to the core problem. The symptoms are only being treated.”
I think ME/CFS is a cardiovascular disorder whether you have POTS or not. I ‘passed’ my tilt table test except that I was as sick as a dog during and afterwords. I’ll bet my money that the blood and circulatory system play a key role in all of this..
Oh, for sure! There is a definite circulatory system problem – but, what triggers that? We have to get down to the “cause” and not focus so much on only addressing the symptoms.
What were your results on your TTT? You realize that some of us POTS people pass it sometimes too. Right? We have good days and bad days and there have been some that will test out okay on certain days and fail miserably other times. I’ve had two of them and both times – failed miserably.
Issie
Somehow I’ll have to find it again. I remember one of my measures was directly opposite my twins (this was a twin study); his went up and mine went down or vice versa.
I didn’t know that about POTS….
Does your twin have CFS too? My nephews are twins too. One was just DX’d with POTS and the other hasn’t been tested yet. The one, sadly is a fainter.
Issie
No problems with my twin except a similar case of vertigo sometimes. The only other connections that I can tell with all this is my mothers difficult case of Sjogrens and her nephew who had MCS decades before anyone knew about it.
Some of us just may have inherited the worst of the genes. (Have you done a 23&me genetic test, yet?) Thankfully, science is advancing and new things are being learned daily. So, your mom had/has sojourns too. My mom probably also has MCAS – Her symptoms are actually worse than mine – but, she hasn’t been officially DX’d with it. Not too many doctors know what they are looking at when they see it. It’s still a new thing and we don’t have enough docs looking into it.
Issie
Some of us question the way that POTS is being treated. There is more coming out about NE levels and salt loading recently.
I think that the way that some are being treated will be taken a closer look at and found to have not been the best long term way of treating.
by Ramakentesh:
Actually some of the ‘hyper’ symptoms can be caused by compensatory adrenalin/epinephrine release and beta receptor supersensitivity.
When NE leaks into plasma as occurs perhaps in NET deficiency its lost to the body and its reception of it – unless its in a sympathetic synapse it has very little effect although there are beta receptors in other sites.
When usually occurs is either the NE gets stuck in the synapse like in the heart and causes tachycardia or it may leak out of the synapse and stop further NE release from presynaptic vesicles causing vasodilation.
Of course in the brain its different.
But Hyperadrenergic/Hyper POTS is just a description of the levels of NE – I dont think it says anything helpful about the primary cause or etiology and sometimes it actually slaps a misnomer in relation to treatment on the condition – Hyper POTS can still have a neuropathic basis etc.
Some docs recently have adopted the neuropathic v non neuropathic POTS delineation which I think is probably more helpful.
If there is dizziness supressing NE might make the person feel worse
By Issie:
But, that jump out of your skin feeling —is the horrible —get your blood to your heart and your head thing that can happen with an increase in NE. NE causes your blood vessels to constrict to try to get the blood from pooling in your limbs and get to the more vital places —heart and brain. As Rama said – it appears there is not proper response to it and there is more release. But, we don’t always handle the release of it in the best way – because emotionally it’s hard to handle. Therefore, my question —if we increase NE would that level out the surges and make the surges more bearable? If there were a more steady stream of NE, would the body eventually balance itself out? If this is a compensatory thing – then maybe – suppressing the response is causing more of a response. There’s just lots of questions that I don’t think we have answers for yet. But, I do think we are closer.
________________________________________________
http://stoppotsvirginia.blogspot.com/2012/04/what-is-causing-your-pots-and-why-it-is.html#.UhbxTeHn9Ms
Claire, did a real good job of listing possible reasons for POTS and the different sub-types – at least those known at that time.
Issie
This is great website – informative, well-written and at times humorous. I love the list of all the different causes.
http://stoppotsvirginia.blogspot.com/2012/04/what-is-causing-your-pots-and-why-it-is.html#.UhvO6dJjt8F
Yes, this is Claire’s website. She has started a new one – called Dysautonomia SOS. She is devoting more of her time to that one. She is a hoot. Very talented. But, also very sick girl with lots of determination to find the answers. It takes all of us to try to get the word out about this. So many of us are searching for answers and being as verbal about it as we can.
Issie
Cort,
I’ve mentioned Ramsays Disease and Dr. Les Simpson’s work trying to bring this to the fore in some other comments before but haven’t found a reply yet. Could it be that the inability of the some of the red blood cells to be able to curl up and thus get oxygen into the smallest capillaries might be involved here?
Suella
My doc feels that it is related to a protozoa that can be spread with mosquito and tick bites – called Protomyxzoa Rheumatica or FL1953. All of the patients that he has tested with POTS and CFS have been positive for this. It lives along with virus and bacteria in a protective field called bio-film. Best way to describe how this works is it forms a shield around it and attaches to the walls of veins. This he feels can cause blood flow issues. Many of us that have tested positive are also positive with other infections that go along with Lyme disease. Working on breaking down this bio-film and allowing the immune system to detect these organisms and go after them, will hopefully make us better. I’ve been in treatment for about 7 months now and am noticing some good improvements. He is in the final stages of getting together his material for a peer review and hopes to be published by the end of the year.
http://protomyxzoa.blogspot.com/2012/07/understanding-protomyxzoa-rheumatica_12.html
http://protomyxzoa.org/