

This overview of the CFIDS Association of America’s webinar on cognition in 2012 was produced while I was with Phoenix Rising but was never published.
We just published Dr. Lapps take on cognition and possible ways to treat it. Now, that we’ve got an overview of the treatment possibilities let’s dive into cognition full-bore with this overview of cognition and ME/CFS by a neurologist, Dr. Lange, and Dr. Vernon, the research director of the CFIDS Association of America.
Cognition, i.e., our ability to think, can be a difficult subject to understand, but Dr. Lange and Dr. Vernon fortunately produced a relaxed, easy to follow webinar.
(This blog, as my blogs tend to do, will present an overview of the webinar, and take riffs off of it. That means that some information in this blog was not presented in the webinar and should not be attributed to Dr. Lange or Dr. Vernon.)
The Cognitive Problems in Chronic Fatigue Syndrome (ME/CFS)
Dr. Lange started off the webinar noting that over 85% of people with ME/CFS report that they have cognitive difficulties and then highlighted some familiar problems:
- Needing to read the same paragraph over and over again to understand it
- Speaking sentences that defy the rules of grammar and logic
- Agonizing decision-making processes
- Heretofore easy to understand conversations taking on an almost algebraic difficulty
Welcome to the world of a person with chronic fatigue syndrome.
Almost everybody with this disorder misses the intellectual sharpness and nimbleness they had pre-ME/CFS. Despite the obvious cognitive problems for people with ME/CFS, however, researchers have had trouble pinning down what’s going on. Dr. Lange went down the list of the usual suspects to start off the webinar.
Central Nervous System Abnormalities in Chronic Fatigue Syndrome
White Spots on MRIs
Those white spots that showed up on the MRIs of ME/CFS patients more than twenty years ago? They’re not the problem; yes, more of them are found in ME/CFS than in healthy people, but far fewer are found than in people with disorders like multiple sclerosis. In addition, they don’t follow a consistent pattern. They can’t be directly tied to the cognitive problems in ME/CFS.
Brain Drain
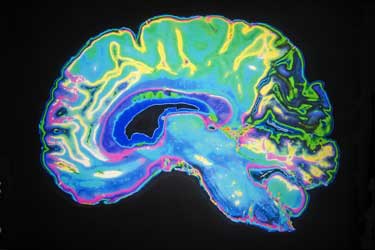
Imaging studies have documented abnormalities in ME/CFS patients brain, but haven’t identified a unique biomarker yet.
Several studies have found reduced amounts of grey matter or white matter in ME/CFS, but others have not. When you control for the presence of mood disorders, the white matter volume losses disappear; i.e., it looks as though they reflect mood disorders more than anything unique to chronic fatigue syndrome.
‘Brain Burn’
The high lactic acid levels found by Shungu (suggesting energy production in the brain has taken a hit) are intriguing, but they’re also found in people with major depressive disorders. They appear to be general indicators of increased inflammation and high levels of oxidative stress. Like the white spots and reduced brain matter, they suggest something is going on–but nothing that is unique to ME/CFS.
Dr. Vernon also said the evidence pointed to ‘subtle’ inflammation – hardly anything that could account for the disability often seen in chronic fatigue syndrome.
Cognition and ME/CFS – What Do We Know?
Functional MRIs
Functional MRIs (fMRIs) show patterns of blood flow in our brains as we do cognitive exercises. They chart an intriguing pattern: they indicate that, given enough time, people with ME/CFS do about as well as healthy controls on all sorts of intellectual tasks–but they take a much longer time to do them; i.e., they have ‘reduced information processing speed’.
Being a bit slower may not seem like a big deal, but if you think how quickly we talk and how many words we have to absorb to understand one another, reduced processing speed could leave one floundering in many environments.
Again, Dr. Lange said the degree of disability in both these area was relatively subtle compared to other illnesses; i.e., she might see a 10 or 15% drop in information processing speeds in ME/CFS but no more, so she sees no smoking gun here either.
Low Blood Flows
After a series of rather lackluster findings, things picked up with the blood flow studies. Not only are they consistent, but the abnormalities tend to cluster in the same parts of the brain. As imaging technology has improved Dr. Lange stated it has improved the validated the existence of low brain blood flows in ME/CFS.
The low blood flow findings make sense given that the orthostatic intolerance seen in ME/CFS largely results from reduced blood flows to the brain upon standing. Note, though, that the blood flow studies are done with patients lying down, and consider how much more significant the blood flow reductions to the brain might be if they were observed with the patient standing. (One of the CFIDS Associations studies is doing just that.)
HOWEVER, while the brain blood flow findings were consistent, they were not terribly abnormal and, again, they do not appear to be unique to ME/CFS. The same low blood flows across the front part of the brain occur in mild traumatic brain injury and other disorders.
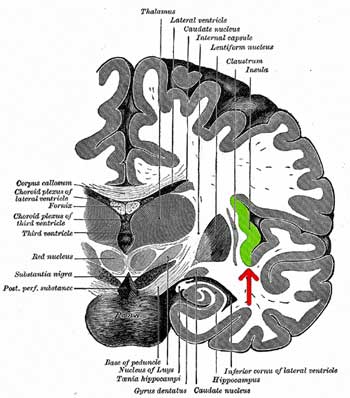
The Brain Regions Affected in ME/CFS Show Promising Consistency
When looked at in total, the neuroimaging findings showed a promising consistency with the same parts of the brain – the insula, thalamus, anterior cingulate and hippocampus – showing up again and again. These sections of the brain work together, and most influence a hot topic in ME/CFS research right now: the autonomic nervous system (ANS). The ANS controls the heart rate, blood pressure, blood flow, regulates the immune system, and plays an important role in cognition and emotions.
These same brain areas are also showing up again and again in chronic pain disorders such as fibromyalgia, interstitial cystitis, and IBS. Check out some of the things these parts of the brain do:
- Thalamus – regulates sleep and alertness, processes and relays sensory information, regulates ‘arousal’, level of awareness, motor signals. (Thalamic or Dejerine–Roussy syndrome, which causes allodynia and hypersensitivity to pain, and is caused by reduced blood flow to the thalamus)
- Insula – regulates homeostasis (ANS), awareness of body states, pain, perception, motor control and exercise regulation, speech articulation, vertigo, immune regulation
- Anterior cingulate -affects the autonomic nervous system, cognition, emotion, error detection
- Hippocampus – short and long term memory, spatial perception, very vulnerable to long term stress
Problems in these brain regions could play a role in sleep and alertness problems, the increased ‘arousal’ (i.e., fight or flight), increased pain and body sensations, exercise issues, loss of verbal abilities, vertigo, autonomic nervous system problems, memory, the stress response, and even immune problems in ME/CFS.
The Gadfly Speaks….
Consistent results suggest the researchers are on track -a very good thing – but, as she often does, Dr. Vernon – a stickler for rigorous study design and a leader in the march for research standards in ME/CFS – ticked off a rather long list of potential problems with study design. (One researcher told me rather bluntly that study design in CFS tends to be ‘terrible’.)
Some of the problems Dr. Vernon cited included very small sample sizes, not applying the CFS definition rigorously, not taking into account co-existing mood disorders, lack of disease controls, an excessive number of different neuropsychological tests used making it difficult to compare study results, etc. In fact, so many different neuropsychological tests were used in these studies (dozens), that it almost appeared researchers went out of their way to use a unique test…
It seemed like almost couldn’t be worse in that regard, but there is some good news. The research community does recognize this problem exists, and ‘gold standards’ are being developed. Once the research community gets on the same page, the study results should be more ‘meaningful’ and the field should progress more quickly.
Conclusion
If you’re looking for a biomarker- something unique ME/CFS – these studies have failed to provide one. If you’re looking for evidence of central nervous system problems abnormal findings have been found in several areas of the brain. They’re not, however, the kind of dramatic abnormalities that the rates of disability and distress in chronic fatigue syndrome tell us must be there – somewhere in ME/CFS. A Japanese study has found abnormalities that may take us closer to the heart (or brain :)) of ME/CFS, and we’ll cover that in Part II.
That the same brain regions are showing abnormalities across multiple studies, however, suggests researchers have identified core parts of the brain that have gone awry in ME/CFS.








Cort,
Excellent article, thank you for putting this piece together. I wonder how those of us with a partial empty Sella (and Male & skinny) relate to these regions of the brain being impacted.
Thanks
With Empty Sella, I find it is especially to treat for hormonal deficiencies, not relying on the lab normal ranges, but rather based on the person’s symptoms and reponse to treatment with the hormones
I’m new here i have fibro and all of what was mentioned in the article. Help me
I’ve always thought, with my own case of CFS, which included the brain fog and also bloated gut problems, that the ANS is the key. I still believe that, but now even more stronglhy.
Me too; my gut issues and orthostatic intolerance issues have gone hand in hand. I just feel the ANS and the blood vessels are a major part of the problem….Thankfully – of what limited research there is in ME/CFS – the ANS is getting some good attention.
Thanks, Cort. Looking forward to your next installment.
same brain regions may be involved with dementia. Coincidence?
Thanks Cort.
By the way, Gudrun Lange isn’t a medical doctor so I’m pretty sure can’t be called a neurologist. A “neuropsychologist” might do the trick.
Thanks Tom
I looked her up – yes, she’s a clincal neuropsychologist and a professor.