

“I don’t want anyone to go though what I had to go through.”

Lauren Stiles story with dysautonomia began in a familiar way – a sudden, mysterious and debilitating decline
(Athletic and healthy, Lauren Stiles was suddenly felled by a mysterious illness in the middle of ski trip that left her unable to walk. It took years, but Lauren’s doctors ultimately found that an autoimmune disease had attacked her autonomic nervous system, which had resulted in the symptoms of dysautonomia. Not wanting anyone else to go through what she did, Lauren created Dysautonomia International in order to bring attention to a prevalent but under diagnosed condition.
Many studies have documented autonomic nervous system problems in ME/CFS/FM. From postural tachycardia syndrome to blood flow problems to muscle issues to poor blood pressure regulation to sleep and the emotions the ANS is showing up again and again in chronic fatigue syndrome and fibromyalgia.
Now, to celebrate Dysautonomia Awareness Month, Lauren Stiles gives us a tour of the complex world of autonomic dysfunction – one many doctors are unaware of – in Dysautonomia 101 for ME/CFS/FM)
What is Dysautonomia?
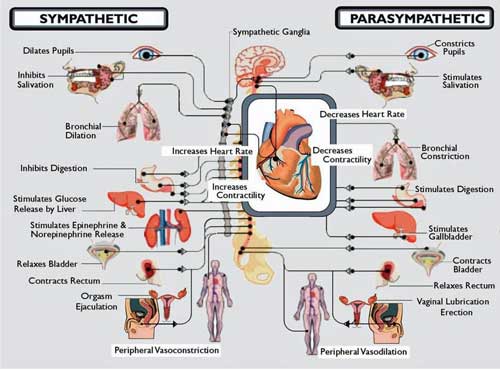
Dysautonomia is an umbrella term that means any dysfunction of the Autonomic Nervous System (ANS). The ANS controls the involuntary functions of the body like heart rate, blood pressure, breathing, digestion, sweating, kidney function, dilation and constriction of the pupils and more.
One reason dysautonomia is under diagnosed is because it can cause so many different symptoms (Copyright (c) 2012 Vinik)
When there is damage to the ANS, or if it is not functioning properly, a person can experience symptoms impacting any one or more of these bodily systems, and sometimes all of them at once.
Common symptoms of dysautonomia include lightheadedness, fainting, dizziness, shortness of breath, chest pains, abnormally low or high blood pressure, abnormally fast or slow heart rates, palpitations, sluggish pupils that don’t constrict properly, which can cause headaches and sensitivity to light, gastrointestinal motility problems, which can result in diarrhea, constipation, bloating, feeling very full after meals, reduced or sped up movement of food through the GI tract, bladder dysfunction, which can cause a person to have to go often or to have trouble emptying their bladder, problems regulating body temperature, which can make a person very sensitive to warm or cold environments, excessive or reduced sweating and much more.
Not every person who has dysautonomia has every symptom, and not every symptom on this list is always caused by dysautonomia. Additionally, not every malfunction of the ANS means a person is “sick” with dysautonomia. For example, fainting is usually caused by a temporary imbalance in the ANS, but fainting once or twice in your life is pretty common, even in totally healthy people.
Is “Dysautonomia” a Disease?
No, “dysautonomia” is not a specific disease or diagnosis. If your doctor has told you that you have “dysautonomia,” ask your doctor which kind of dysautonomia you have, or what’s causing it. There are a number of different medical conditions that are considered to be primary forms of dysautonomia, such as:
- Neurocardiogenic Syncope
- Postural Orthostatic Tachycardia Syndrome (POTS)
- Autoimmune Autonomic Ganglionopathy
- Pure Autonomic Failure
- Multiple System Atrophy
- Baroreflex Failure
- Familial Dysautonomia
Family Matters
It is important to note, having relatives who also have dysautonomia symptoms doesn’t mean you have “Familial Dysautonomia.” Familial Dysautonomia (“FD”) is a very specific inherited form of dysautonomia that only impacts about 350 people in the world. It is seen in people who are born to two Ashkenazi Jewish parents who both passed on a specific gene mutation. FD patients usually have severe disability from the time of early childhood, and often have developmental problems and distinct facial characteristics. While there have been advances in the treatment of FD that prolong life, FD patients often do not survive beyond 20-30 years.
If you have dysautonomia and another relative does too, it is very unlikely that you have FD. Many other primary forms of dysautonomia can run in families, such as Neurocardiogenic Syncope and Postural Orthostatic Tachycardia Syndrome. Additionally, there are secondary causes of dysautonomia, explained below, that can also be passed down through families – such as diabetes or Sjögren’s Syndrome.
Secondary Forms of Dysautonomia
Secondary forms of dysautonomia are diseases and conditions that don’t always cause dysautonomia, but can in some cases. For example, diabetes is not considered to be a form of dysautonomia, but if diabetes causes damage to the autonomic nerves, as it does in about 20% of diabetics, it can cause the symptoms of dysautonomia. Doctors call this Diabetic Autonomic Neuropathy.
Many other underlying diseases and conditions can cause damage to the autonomic nerves which results in dysautonomia symptoms – Pre-Diabetes, Sjögren’s Syndrome, Lupus, Anti-Phospholipid Syndrome, Multiple Sclerosis, Parkinson’s, Lyme Disease, HIV, Guillain-Barre, Paraneoplastic Syndrome associated with some forms of cancer, certain chemotherapy and other drugs that can cause autonomic nerve damage, vitamin deficiencies, heavy metal poisoning, alcoholism, mitochondrial diseases, genetic diseaes and more.
This is why it is so important to see an experienced autonomic specialist if you have symptoms of dysautonomia. Identifying and ruling out potential underlying causes can be a complicated process, and make take the expertise of several specialists in different fields.
In some cases, no underlying cause of the autonomic neuropathy can be found. This would be called “idiopathic autonomic neuropathy” or “idiopathic dysautonomia.” Some doctors use the terms “autonomic neuropathy” and “dysautonomia” interchangeably. Autonomic neuropathy means that the autonomic nerve fibers have been damaged. Dysautonomia can refer to the damage that has occurred to these nerves. Dysautonomia can also refer to a malfunction of the Autonomic Nervous System when the autonomic nerves fibers are intact.
Is Dysautonomia Rare?
Nope! Dysautonomia might not be well known, and might be misunderstood by a majority of the medical profession, but it is not rare at all. Some of the primary forms of dysautonomia are considered rare diseases, such as Familial Dysautonomia, Autoimmune Autonomic Ganglionopathy and Multiple System Atrophy, but other forms, such as Neurocardiogenic Syncope and Postural Orthostatic Tachycardia Syndrome (POTS) are relatively common.
Dr. Philip Fisher, Chairman of Pediatric and Adolescent Medicine at the Mayo Clinic, is a prominent POTS researcher. He has estimated that POTS impacts about 1 out of every 100 teenagers. Looking at the 2010 Census data, this would equate to just about 500,000 teenagers having POTS in the US. We know that POTS impacts adults as well. Other experts estimate that POTS impacts between 500,000 and 1,000,000 Americans.
Of course, POTS is not just an American problem. As awareness increases within the medical profession, people are getting diagnosed with POTS all over the world and POTS research is now occurring on several continents. If we used the conservative estimate of 500,000 Americans having POTS, and if we assumed that the same percentage of the population was impacted worldwide (which may or may not be the case), that would mean that roughly 11 Million people on planet earth have POTS. The number would double if we used the higher 1,000,000 Americans estimate.
While the precise statistics have not been determined yet, it is clear that POTS is not rare.
Secondary causes of dysautonomia are even more common. For example, the 20% of diabetics who develop autonomic neuropathy discussed above translates into 69 Million people worldwide. Dysautonomia was thought to be a rare complication in Sjögren’s Syndrome, until very recently when researchers in the UK determined that over 50% of Sjögren’s patients had dysautonomia.
Perhaps most interesting to the readers of this website, the more dysautonomia symptoms the Sjogren’s patients had, the more fatigue and pain they had as well. Sjögren’s is estimated to impact up to 35 Million people worldwide. If 50% of those individuals have symptoms of dysautonomia as a result of their Sjögren’s, that’s another 17.5 Million people who have dysautonomia. Combining all of the primary and second forms of dysautonomia together, dysautonomia is a very common.
How is Dysautonomia Diagnosed?
“I was misdiagnosed by several doctors, but the disorder causes so many symptoms that it mimics other illnesses,” Lauren Stiles
Some aspects of dysautonomia can be easily diagnosed based on symptoms and a routine office visit exam that includes checking your pulse and blood pressure lying down, and then after 5-10 minutes of standing still. This is called a “poor man’s tilt test.” More extensive work ups can be performed at specialty centers that focus on autonomic disorders. These specialty centers are often staffed by neurologists, cardiologists, or electrophysiologists that have a focus on autonomic disorders.
Check out Dysautonomia International’s World Map to find doctors, support groups and other resources
Autonomic specialty centers use a combination of tools to evaluate patients with suspected dysautonomia. This may include a tilt table test, a QSART (quantitative sudomotor axon reflect test), a thermoregulatory sweat test, radio-labeled blood volume analysis, Valsalva testing, cold pressor hand grip analysis, gastric motility testing, skin biopsies to evaluate small fiber sudomotor nerve density (also called the Sweat Gland Nerve Fiber Density test), pupillometry and other tests. Not every patient will need every test.
While dysautonomia as a whole is fairly common, many doctors are not adept at recognizing it or diagnosing it. Unfortunately, this lack of awareness often causes a lengthy delay from the onset of symptoms to the time of diagnosis. Dysautonomia International’s interactive map provides the name and location of many doctors who have experience diagnosing different forms of dysautonomia.
How is Dysautonomia Treated?
Any underlying condition that could be causing the dysautonomia should be treated, as this will often help improve the dysautonomia symptoms. If no underlying cause can be identified, the goal is to reduce the patients’ symptoms through non-pharmacological methods, lifestyle adaptions, and medication if necessary. The specific treatment depends on the symptoms of dysautonomia that the person is experiencing.
Non-Drug Approaches
Common non-pharmacological measures include increasing salt and fluid intake, wearing compression stockings or an abdominal binder, getting regular reclined exercises like rowing, recumbent biking and swimming (exercise helps build up blood volume, improves hemodynamics, and prevents deconditioning which can make dysautonomia symptoms worse), learning counter-maneuvers that can help prevent a faint from occurring, sleeping with the head of the bead on an incline, eating smaller meals more often throughout the day, reducing intake of refined flours, sugars and other low nutrient high carbohydrate foods, avoiding hot showers, wearing a cooling vest in the summer, and wearing extra layers in the winter.
You can find dysautonomia friendly exercise tips, salty food ideas and products like compression stockings that some patients find useful on the Dysautonomia International website.
Drugs
Medications may be added to help minimize symptoms. The medications used depend on the particular requirements of each patient, but may include beta blockers, midodrine, Florinef, clonidine, Mestinon, SSRI or SNRI drugs (not just for their anti-depressive effects, but for their regulation of neurotransmitters used by the autonomic nervous system), octreotide or Provigil. Outside of the United States, ivabradine is sometimes used instead of beta blockers. Ivabradine is not approved in the U.S.
In urgent situations, IV saline can be used to help increase blood pressure and improve hemodynamics, but experts warn against using IV saline as a regular treatment due to the risks of blood clots and infections that come with any infusion method, particularly PICC lines and chest ports.
Where Can I Find More Information?

Formed in 2012, Dysautonomia International has three offices, an interactive map and an informative website
Dysautonomia International is an all-volunteer 501(c)(3) non-profit focused on improving the lives of people living with dysautonomia through research, education, advocacy and patient empowerment. Our website offers lay person and physician oriented information on many different forms of dysautonomia, dozens of peer-reviewed journal articles, educational videos, patient stories, coping tips, and resources for family, friends, employers and educators.
You can find out about the latest dysautonomia related news, events and research by “Liking” our Facebook page, www.facebook.com/dysautonomiainternational, and following us on Twitter @Dysautonomia. You can also find dysautonomia related support groups, awareness events, meet ups, and doctors who specialize in autonomic disorders on the Dysautonomia International Interactive Global Dysautonomia Map.
- Check out Lauren’s story – “From Chronic Fatigue Syndrome to Fibromyalgia To POTS To Success: One Woman’s Journey Through the Medical Profession”.
- Check out Lauren’s story in a Newsday article
Dysautonomia Awareness Month
This October has been the second annual Dysautonomia Awareness Month. While you’re “thinking pink” for breast cancer awareness each October, don’t forget to “make some noise for turquoise!” Turquoise is the color used by Dysautonomia International and several other groups to represent dysautonomia awareness. This past month volunteers from around the world have been holding dysautonomia awareness activities, fundraisers, and educational events to help spread the word about dysautonomia.











Thank you for a fine article on one of my favorite topics. I have collected some references here:
“Autoimmune Autonomic Neuropathy”
http://www.followmeindenmark.blogspot.dk/2013/09/autoimmune-autonomic-neuropathy_23.html
Thanks, Helle – there’s so much to explore in this topic.
I noticed that you highlighted this study – http://www.ncbi.nlm.nih.gov/pubmed/17352367 – in that page, which suggests that about nerve damage appears to be present in about half of the POTS patients seen at the Mayo clinic over a considerable amount of time, and that a substantial percentage of that may be due to autoimmune processes – very similar, it sounds, Lauren’s experience.
POTS is so complex, complicated and difficult. As a person that has had POTS most of my life – trying to find “bandaids” to help with our issues is difficult. The more awareness that we can get out there —the better.
I personally question a lot of the “traditional treatments” used for most POTS people. But, at least there is more awareness happening and some other doctors are looking into “cause” and “treatment” for us. I’m having good success with a diet change and addressing protozoa. That seems to be helping my POTS more than anything else I’ve done over the years. Of course, this treatment addresses the immune system. That could be the key to all of our issues —autoimmune dysfunction.
Thanks for trying to get our stories out there. As the more verbal we are, the louder we shoot —someone that maybe can help —-might hear us and be able to put their energies into uncovering more solutions for us.
Issie
Given all the ways POTS and autonomic nervous system problems – including small fiber neuropathy – can be caused, and the many different things they throw at it to fix it – I’m not surprised to find new treatment possibilities show up – and when they show up – particularly in a disease like this which is not well studied – they often come out of the offices of doctors who are trying new things. They’re the ones that really doing the experimenting.
It is really exciting to find these “pioneer type” doctors that are willing to look further than the obvious and find things that we may not suspect and the treatments help us in other ways. Those type of doctors are hard to find and also take a lot of abuse from their peers and some patients that want to disagree with their treatments. But, the “proof is in the pudding” – so to speak. If it works —then there is no denying that.
I’ve been pretty verbal about what I’m doing and how it’s affecting me. It’s really interesting to me how people will criticize something when it is different than what is considered the “norm”. I’ve taken a lot of criticism just from telling my experience – sad to think what the doctors themselves hear. You have to admire someone who sticks to their guns under such adversity.
It takes someone with another idea and then research to either prove or disprove something. And then it takes time for others to get on board with something that is new. Todays ideas are tomorrows facts.
Issie
Ha! The louder we shout – not shoot. LOL!
Just a bit of encouragement to those that have POTS. I’m in a flare with my back right now. Got sent to a Spinal Rehab Doctor today. Guess what? He HAD POTS. Was DX’d at Vandy and was so bad he had to move in with family to care for him. He was nearly incapacitated. He started going to my Doc. and treating the protozoa with low dose antibiotics and started the low-fat, whole food vegan diet. He has been doing this for 3 years now. He says he would now say he HAD POTS. At times he is dizzy if he stands too fast, but no longer has the tachycardia and things that go along with POTS. He encouraged me to stick with my diet and the protocol I’m on. He really thinks our doc’s ideas and protocol is the right way for us to go. It addresses the immune system, and targets the biofilm and pathogens that live in it. It was a nice surprise to meet him and to see that someone can get over POTS. At least he feels that he no longer has it. He speaks of it in past tense. He had to stop practicing as a doctor when he got it and now is very functional in his life.
It has definitely been the best thing I’ve done. I’ve tried all the meds and assistance (compression hose, ab binders, raising bed etc.) that the doctors tell us to do. But, this is the first thing that is really making me see improvements. I’ve been on this for 8 months now. Since I do have autoimmune things going on and lots of other things with MCAS and EDS connected —it will take time. It’s not a quick fix. But, I intend to stick with it. It’s too much of a difference to change anything. To think —–DIET may be our key. And addressing autoimmune and inflammation issues is a big part of that.
Issie
Glad to hear that. How are your lab readings doing? Is the doctor checking autoimmune/immune factors. Any change there.
All my labs are looking better. I was in Chronic Kidney Disease stage 3 and am now almost in stage 1. My blood sugar readings are from pre-diabetes to completely normal. I got my Vit D levels to finally come up. All my lab numbers are greatly improved.
As for autoimmune, still having issues there. So, waiting for that to get better. I was told it would take time. Not something that will happen over night.
But, seeing the labs and the science showing improvement and just knowing that I’m functioning so much better —to me, is proof enough. I was in a wheelchair for over 6 months and could barely function and now I’m preparing to go on vacation to Hawaii for a couple of weeks.
Issie
Can anyone please tell me what sort of specialist Dr one would see to investigate Dysautonomia? I live in New Zealand and have had type 1 Diabetes for 30 years and my Endocrinologist doesn’t even believe there is such a thing as CFS and simply dismisses my requests to attempt to find ANY diagnosis for me by saying everything is attributed to Diabetes and to just accept at 44 years of age this is my lt. Not so! Any advice would be appreciated thank you.
Dear Vanessa,
Diabetes is the most common cause of autonomic nerve damage, and thus, is the most common cause of dysautonomia symptoms.
If you have diabetes and symptoms that sound like dysautonomia, there is a good chance that your diabetes has damaged your autonomic nerve fibers. Ask your diabetes specialist about diabetic autonomic neuropathy. There are several ways to test for it – some are mentioned in the article.
There is a cardiologist interested in dysautonomia located in Christ Church, NZ listed on the Dysautonomia International map: http://www.dysautonomiainternational.org/map.php
If you can travel, the Baker IDI in Melbourne, Australia is one of the world’s leading diabetes and dysautonomia research centers.
There are symptomatic meds that may help with dysautonomia symptoms, but if diabetes is causing it, the best way to treat it is to carefully control your diabetes as best as possible.
Good luck!
Lauren Stiles
Dysautonomia International
Thank you Lauren for your prompt reply which I will follow up 🙂
i had the same problem. was in hospital for about a week. kidney failure and a unknown virus that cause the problem. since then i’m tired all day long, cant eat and feel sick te the whole time.and the docters – well, not very helpfull!!!!
By the way dysautonomia was incorrectly spelled in several of the headings. That was my mistake – I added some headings – not Lauren’s.
Thank you for this excellent overview of dysautonomia, Lauren!
-N
What about the Driscoll theory on YouTube?
Mast cells? Interesting stuff
Sounds like a good blog Diana….Let me know if you’re interested in doing one and informing us. (Mast cells are nothing if not interesting :))
Mast cell problems do seem to play a big part with some of us. Interesting enough when I added GastroCrom to my H1 and H2 it greatly improved my POTS symptoms.
I tried the protocol that Dr. Driscol recommended with Diamox. I tried this before going on my diet. This made me sooooooo SICK. It was absolutely the wrong thing for me to do. Not only is Diamox a sulfa drug and I have a CBS mutation, but it is really hard on your kidneys and I have CKD. Most of the friends of mine that have tried this —have all stopped it. It made us all worse. I know some seem to be getting help from it. But, this is really hard on your body. We are already dehydrated and this seemed to make things worse for me.
I appreciate the “Theory”, but don’t think it explains everything. There probably is an issue with CCVSI – but for different reasons than is proposed by this “theory”. (Just my opinion – not trying to start an argument.)
Issie
This is a very well written article. I was surprised and disappointed that biofeedback was not mentioned as a form of treatment. My daughter suffered for five months, homebound and wheelchair-bound, with POTS. Biofeedback is what normalized the function of her ANS and gave her her life back!! She has been one year symptom free. Stories like hers are very, very typical at the POTS treatment center in Dallas, TX. Biofeedback saved my daughter. Others should know this, especially Dysautonomia experts.
Glad to hear your daughter improved so much. I haven’t heard of biofeedback being used either, but dysautonomia can arise in some many ways I’m not surprised it can – in different people – be attacked in different ways. I have heard that the autonomic nervous system is more amenable to control than other systems; maybe she was able to calm down the system enough to allow it to reset?
Wow!
I have all these symptoms. M.E. is my primary diagnosis. Following your blog with interest … thanks!
Haiku: “Although normally – dysautonomia is – unseen, its not rare”
A dysautonomia Haiku – I love it 🙂
That was great Neil!
CORT , SEGUIDORES DE ESTE SITIO EN TRATAMIENTO HAY ALGUNAS CITAS EN LA LITERATURA MEDICA QUE 600 MGR DE ACIDO ALFALIPOICO CADA 24 HR Y COMPLEJO B
MEJORA LA DISAUTONOMIA Y EN MI CASO MEJORA ADEMAS MI FCS
Well I wish that I had stumbled across this post earlier, because I would have been interested in writing something for Dysautonomia Awareness Month. I don’t recall seeing anything else written about it, but I guess that probably wouldn’t come as too much of a shock to you, especially when trying to compete with “Pinktober” and every company that wants to show it supports breast cancer awareness if you buy their products. It also seems like diagnosing dysautonomia is nearly as difficult as diagnosing fibromyalgia, which would certainly support that there are many unconfirmed cases out there.
Great article! I may be wrong but isn’t dysautonomia diagnosed by an ANS test? I am pretty sure when my cousin was tested the doctored ordered an ANS test to see if there was an imbalance in his body. Any input?
Hi Joan,
I am pretty familiar with all of the testing equipment used by the autonomic researchers and clinicians, and I have never heard of an “ANS test.”
I think, perhaps, you are referring to the ANSAR test? If so, I can tell you that most of the physicians who specialize in autonomic disorders do not consider that to be a credible or diagnostically useful test. There are plenty of doctors who will order it though. If that is the test a doctor is relying on to diagnose or rule out an autonomic disorder, I would find a doctor who has more expertise in how to diagnose autonomic disorders. You can find good autonomic experts here: http://www.dysautonomiainternational.org/map.php
In my own experience, before I was properly diagnosed, I saw a general neurologist who ordered an ANSAR test for me. The results came back “normal,” yet within a minute or two of completing the test, I passed out cold on the floor in the lab. Clearly, not normal. Two years later I found a neurologist that actually specialized in diagnosing and treating autonomic disorders. He used a tilt table test, QSART, Valsalva and other autonomic function tests, along with small fiber nerve density skin biopsies, to accurately determine what form of dysautonomia I had.
You can find out more info about clinical autonomic testing here:
https://www.aan.com/Guidelines/Home/GetGuidelineContent/39
Sincerely,
Lauren
HI all,
Glad to stumble on this website. I have a vague diagnosis of dysautonomia, ha, but clearly I need a new specialist. Any suggestions for firstly good specialists in Melbourne, and secondly, what sort of specialists should I be seeing? I have a cardiologist who has spent the last year doing general cardio workups which are not surprisingly fine (I am a fit 30 year old). I don’t ‘fit’ POTS (postural HYPERtension from 115/70 to 220/190, returning to normal in a minute or two, no rise in pulse rate, no fainting just awful headache and loss of vision) so he has no idea what it could be. I also have tachicardia only during deep sleep (waking up with heart rate 200+ bpm). I have no idea what to do next but I have been fobbed off with this “some sort of dysautonomia” diagnosis. I have had to quit my job and I don’t have private health insurance, so I am on a health care card. Any suggestions? Neurologist next, or try a different cardiologist? Endocronologist? I’m so confused. . .
Hi Jessie. You might want to try to get in touch with Lauren at Dysautonomia International. She might have some good ideas for you. Good luck!
Hi Jessie,
Try getting in to see Murray Esler at Baker IDI. He’s a cardiologist, but has substantial autonomic expertise and can probably perform tests to pinpoint more accurately what kind of dysautonomia you have. You can also try finding an autonomic neurologist. Esler’s office may be able to recommend someone.
You also might want check in with Michele from the LivingWithBob(Dysautonomia) blog. She’s a lovely Aussie who has a great neurologist that has finally uncovered the root cause of her dysautonomia.
Regards,
Lauren
Hi Lauren.
I have severe POTS (my heart rate can increase up to 65 beats per minute on standing). Those who have hyperadrenalic kind of POTS like I have get high BP on standing (mine can jump from 130 to 170 in one minute of standing) and if bad enough also may need saline IVs.
Ive had to have saline IVs in hospital when my POTS is very bad and my BP went then up to 180 over something due to it (my LOWER reading can get up to almost 140 when up on feet.. severe hypertension). Dr David Bell has given saline IVs to some of his POTS patients who have high BP flare to get the BP down. This can quickly help me too and without this I will suffer from a bad POTS flare up no matter what the trigger (heat or being upright too long) for days.
Last time I had to be ambulanced to hospital due to the POTS resting heart rate had gone up over 140/150, BP 180 something..and a major collapse and I ended up dehydrated to.. I do not hold my fluid well and what I drink with the POTS just seems to be peed out, thou Florinef does help some. My blood tests came back showing my kidneys were in trouble… I was given 2 bags of saline to try to boost my blood volume, get my BP and heart rate down and to help me over the crash I had with the POTS. (It had been a hot day and my body can not handle getting too warm, I can get sick due to this even at temperatures normal people find pleasant but this day was a bad one).
In this article you said.
“In urgent situations, IV saline can be used to help increase blood pressure and improve hemodynamics”
.. anyway Im just pointing out that its also used in some cases of POTS when BP goes up very high due to the POTS, to help get the BP DOWN! and I can say that IV works very well. I wish that was noted in this article too as I do come across quite a few others with ME who do have the orthostatic hypertension kind of dysautonomia with the POTS.
Lauren,
This article is great and extremely detailed, but it seems that some people are taking away that “secondary forms” of dysautonomia are the same as “types” of dysautonomia. I recently saw a blog claiming that fibromyalgia is a *type* of dysautonomia.
Could you clear this up, please? My understanding from my doctor (Daniel Clauw) is that, in the long term, fibromyalgia (now known to be a neurogenic condition) damages the autonomic system, causing symptoms of dysautonomia. What is your take on this?
I’m afraid I don’t know the answer and I wonder if anyone does. Clauw could be right or dysautonomia could play a more central role. Clauw believes everything derives from the central nervous system; others believe problems with the peripheral nervous system play a major role. I’m a laymen but I just don’t know if a conclusive answer is present.