

My ME/CFS History
1989 – The First Flu-like Illness
I was always a high energy burn the candle at both ends type-A person. In my early twenties (1989) I came down with a flu-like illness that did not go away. I had gone from a person who would play sports 4-6 hours a day, to one who would get worn out walking around the block. The doctor’s said I had mono or Epstein-Barr Virus (EBV), but the condition did not resolve.
At first I vowed I would solve the illness but then I became depressed and took a leave of absence from work and just slept and read all of the classic novels. Six months later my roommate got tired of me being depressed and laying around the house and we got into a fight that more resembled a wrestling match which snapped me out of my funk and I found I was normal again.
Circa 1997 – Giardia and Intestinal Issues
I then returned to my high energy ways. Eventually, I took time off to travel the world and got dysentery and giardia. I was given the standard drugs to kill everything but my GI system would remain a mess and conventional medicine found nothing wrong. This was about a year before my next set of issues.
Circa 1998 – Stress, A Flu-like Illness and Orthostatic Intolerance
I had a lot of stress in my life and came down with a flu-like illness which went away, but I was left with a lot of neurological issues that the doctors could not find an answer for. Eventually, I did a tilt table test and was diagnosed with neutrally mediated hypotension and ME/CFS. At that time my symptoms did not meet the current defined definition for Chronic Fatigue Syndrome.
I was put on Paxil and Florinef and on that combination I lead a relatively normal life for about ten years. I generally was a happy person who loved doing things and living life and still had lots of energy. I would just have bad days and I could not point my finger as to why. Nobody suggested that I should have gotten off of the SSRI’s.
Circa 2006 – Stress, Depression and Sleep Problems and Reduced Ability to Exercise
Eight years ago, I became excessively stressed out and depressed again, but I did not lose my energy. Instead it affected my sleep. I was taken off Florinef and put on Celexa. Again, I recovered and was leading a relatively normal life but my exercise tolerance was decreasing. I was in general a happy person but was feeling limited and somewhat trapped. My sleep was still somewhat fragile.
Then work conspired to screw up my sleep by putting me on-call nights and working days and I went almost 2 weeks without sleep leaving me in a worse state, but still I had energy and was able to go to work. Eventually, I overcame that period but my physical limitations had increased. I was still able to exercise some and live a relatively normal, but constrained life. I had a good PC doctor who was working with me on the Teitlebaum’s advice, and I was working with Dr. Nancy Klimas out of the University of Miami.
About 3 years ago, my primary care doctor died of a brain tumor and Dr. Klimas and Dr. Rey left University of Miami and stopped taking insurance, so, I was left treating myself. I was frequently frustrated by my physical limitations and found that if I pushed too hard, I would have a bad day or 2, but then I would bounce back.
Around the summer of 2012, my company put up a basketball court in the back parking lot. I started increasing my exercise and playing a little basketball with the usual result that the days I overdid it, usually meant 1-2 days where I felt not so great, but I still remained 70 – 80% functional. However, I figured it was worth it to do the things I loved to do, even if it cost me a few rough days.
Meanwhile, I ignored the other signs that things were getting worse. I was having more anxiety issues and I was sweating through 3 shirts a day at work. In December of 2012, I did some blood tests that showed I had elevated creatine kinase (CK) levels (not too elevated 200 – 500) and a positive ribonucleoprotein (RNP) test suggested an unspecified autoimmunity issue).
2013 – the Race and the Collapse
Then I decided to do this Superhero race in January 2013 which was a 5 mile obstacle course race. I was feeling crappy before the race, but went on and quite enjoyed myself. Three days later I came down with flu-like symptoms. A week after that I was having a panic attack and my life went steeply downhill for the next 8 months.

It was the race though that put Chris down. He got through it fine but three days later collapsed -and went on collapsing.
My sleep was a mess and I was living off adrenaline to cope with the doctor’s visits. One psychiatrist put me on Seroquel 25-50 mg to help with my sleep. This worked at first but left me feeling flat. Then my energy left me completely and I felt like I was a 90 year old. I could not even walk around the block.
There were several times when I did not sleep for 72 hours and felt so weak, that I thought I would die. In June, a few days before my daughter’s 7th birthday, I was still a mess but for some reason that afternoon, I felt a little better. I started helping organize the yard for the party, I had a little adrenaline going and must have pushed too hard. Two days later, my right foot had gone numb and I was becoming severely depressed. The day of my daughter’s birthday was incredibly difficult and I spent most of it in bed.
I have been in survival mode ever since. My biggest issues were depression, brain fog, sleep, anxiety and fatigue. I also had all the classic CFS immunological issues such sore throat, swollen glands, and headaches. I was living in a fog where I felt trapped inside my own body and brain. My depression was not related to my limitations but was a biochemical imbalance that left me in a place where I could not experience happiness and I sometimes felt that I would be better off dead.
Also, I was experiencing what I called attention deficit disorder (ADD)on steroids. It was hard to focus on any one thing for very long and I functioned best by jumping from one menial task to another. Other issues that occurred included blood sugar dysregulation, and muscle wasting in my foot and jaw.
Much of that has now improved. I currently have enough energy that I could function in the real world if not for fatigue and the neurological issues.
What I Know From Medical tests.
My immune system is/was not functioning very well –my NK cells are low. I have a reactivated HHV-6 and HCMV infection. My blood sugar is borderline diabetic – elevated fasting glucose and A1C. My testosterone is low and does not respond to testosterone gels. My 24 hour cortisol test is high. My blood pressure is borderline high and fluctuates. I have an elevated CK levels but not too high to indicate a specific diagnosis. I don’t have sleep apnea or restless leg syndrome.
Why Dr. Cheney?
For several reasons.
- I was feeling desperate after Dr Rey told me that she could do nothing else for me, and sent me off to try Rituxamab or GcMaf with doctors that had no experience with those drugs.
- I watched a video which Dr. Cheney talked about the heart issues – which I had experienced – which Dr Cheney said were improved with VIP spray.
- Dr. Cheney puts his patients on B-12 and Mg injections which was the next thing I wanted to try.
- Dr. Cheney was working with other doctors, Dr Brewer, Dr Shoemaker, and Dr Kane who were looking at similar conditions and using different treatments.
- Dr. Cheney had already experimented with stem cells and GcMaf and had experience with both related to CFS.
The First Visit
I just returned from my trip to Asheville, North Carolina to see Dr. Cheney.

On the plus side, Asheville is a great little city situated on the Blue Ridge Parkway along the Appalachian Trail. Along with being an outdoorsy city, it also contains a large contingent of people who are either stuck in or trying to relive the 60s (very bohemian), and this gives the place a lot of character. There are also lots of good restaurants.
The weather was cold and there was even a dusting of snow one morning, but it was nice to have some cold weather as I had come from Miami.
The Heart and the Mitochondria
Dr. Cheney has very specific ideas on what causes the symptoms of CFS. He believes a breakdown in the mitochondrial process that converts food and oxygen into energy (ATP) and water is a key factor. He also believes if mitochondria were not disrupted the person would die from oxidative stress, and that the mitochondrial ‘breakdown’ is a compensatory response that keeps that from happening.
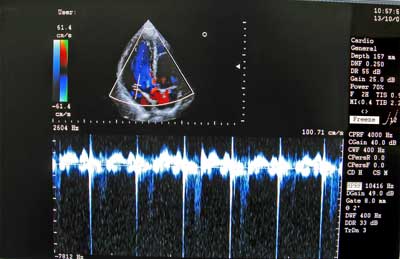
Dr. Cheney believes the reduced cardiac filling he sees is a compensatory and life-saving response to mitochondrial dysfunction associated with increased oxidative stress. the doppler image is on top.
Dr. Cheney uses his state-of-the-art 3D echocardiograph machine at his office to measure the IVRT, or isovolumetric relaxation time. The IVRT is an interval in the cardiac cycle that extends from the time of the closing of the aortic valve to the opening of the mitral valve. During this time interval, the heart muscle around the left ventricle (the main pumping chamber of the heart) relaxes so that the left ventricle can expand and take in a new batch of blood. In a normal healthy person, the IVRT is about 70 milliseconds or so.
Dr. Cheney reports that nearly all his patients have significantly longer IVRT’s. The rate at which the heart muscle can relax is limited by its supply of ATP. So if there is mitochondrial dysfunction, and ATP levels are low, then the heart muscle will relax more slowly than normal, and the IVRT will be longer than normal. That will leave the left ventricle unable to fill completely during the time interval available before the next contraction. The result is that the stroke volume, and hence the cardiac output (blood pumped out per minute by the heart), is lower than normal. Dr. Cheney refers to this as Diastolic Dysfunction.
He uses the IVRT measurement to determine whether a treatment modality has a positive or negative effect. If the treatment modality decreases IVRT increasing cardiac output, then it is good. If it makes it worse, then it is bad. For example, giving oxygen to CFS patients is bad as it increases the IVRT. Dr. Cheney believes giving a person with CFS more oxygen puts a broken energy system into overdrive causing them to feel worse.
Low Blood Volume
Low blood volume is another common issue in ME/CFS. Dr. Cheney believes the low blood volume results from central diabetes insipidus (not to be confused with diabetes mellitus, which involves blood sugar and insulin).
Central diabetes insipidus is caused by insufficient secretion of antidiuretic hormone (also called vasopressin) by the hypothalamus/pituitary. Lower than normal vasopressin levels cause the kidneys to excrete too much water from the blood into the urine, causing larger than normal daily urine excretion in ME/CFS patients (normal is about 1.5 liters per day).
This causes constant thirst, and the desire to drink more fluids than normal. Even added fluid intake, however, is unable to keep up with large losses of fluids into the urine. The low blood volume (hypovolemia) that results causes the flow of blood back to the heart (venous return) to be lower than normal. Since the heart can only pump out as much blood as it receives, this is another factor that causes the cardiac output to be lower than normal in ME/CFS.
HPA Axis Dysfunction
HPA axis dysfunction also impacts the circulation in ME/CFS. Normally, the HPA axis plays an important role in regulating blood pressure, but when the HPA axis becomes dysfunctional, as in ME/CFS, the blood pressure usually drops lower than normal.
Intracellular Magnesium/Potassium Deficiency
Finally, in many cases of ME/CFS, Dr. Cheney finds a deficiency of intracellular magnesium or potassium or both. These two minerals are important for maintaining a steady heartbeat (sinus rhythm). If one or the other becomes deficient, arrhythmias or palpitations can occur.
The low blood pressure, the low blood volume, the diastolic dysfunction, and the heartbeat problems all make it difficult to deliver normal blood flow to the various parts of the body — especially the brain when the person is upright.
This combination of problems results in a variety of unpleasant conditions such as orthostatic hypotension (OH) and postural orthostatic tachycardia syndrome (POTS). It also causes symptoms such as fainting in a warm shower, pooling of the blood in the legs, and palpitations. POTS (tachycardia upon standing) is caused by the efforts of the sympathetic nervous system to increase the cardiac output in the face of a low stroke volume.
Below is what Cheney had to say on the subject.
“All my career, I have been trying to answer the question of what do ALL CFS cases have and at least most healthy controls do not have. I have come up with only two. All CFS cases are toxic to oxygen by echo derived IVRT response criteria as against 1/3 of healthy controls who are mildly toxic to oxygen (but when probed carefully are not as healthy as they purport to be. (i.e., “I used to run a mile until I got mono in HS, and ever since then I can no longer run a mile but I am healthy.”
The cause of oxygen toxicity is likely to be poor redox control which will lower the SED rate due to chronic oxidative injury to the RBC membrane. Dr. Cheney states data from Kennedy-Krieger Labs in Baltimore as well as membrane pictures from John McLaren-Howard in the UK provide ample evidence that that has happened.
The other problem that appears to be universal in “disabled” cases of CFS as distinct from the walking wounded with CFS is low cardiac output with a cardiac index (CI) of less than 3.0, where normal is 3.0-3.5. Cheney says, “I have yet to see a 3-D CI above 2.8, and the average is 1.8 in my practice which sits at the cardiogenic shock threshold. This is nothing short of incredible. Physiologic data such as the cardiac index is fundamentally a much better clinical correlate than any lab marker.“ Mine is currently 2.5.
As noted above, Cheney believes the low cardiac output is a compensatory response to poor redox control (i.e. oxidative stress) and that without that people with ME/CFS will die. He notes that he finds abnormal redox tests (low GSH/GSSG ratios or low NADPH or low SOD or GPx function) with greater predictability than any of a host of immune markers.
Treatments
He has given me a list of things to try. Some are cheap and relatively easy, but others are more expensive and seem a little far-fetched. Based on my testing with him, and my relatively low number of other symptoms, he believes I’m in the group that usually sees some benefit from his treatments.
It will probably take me 6-12 months to work my way through these treatments and see how they will affect me. Some, he warned, will most likely make me feel worse at first (and I’m not really looking forward to that!).
So was it worth $10,000? If I actually do all of the treatments and the labs over the next year, it will probably cost me another $10,000. Thus, my answer to the question is, maybe. If I can reach a higher level of functionality and maintain it, then yes. Since I really believe Dr. Cheney is on a mission to understand and fix this illness by using scientific reasoning and data-driven analysis, I am glad to have him on my team.
- See Part II – Dr. Cheney’s Protocol












what makes the rx so expensive?
what exactly will be done for $20,000
I live in the Asheville area is the dr still in this area?
does medicare cover any of the rxs?
I will be anxiously waiting for your reply
I have had fm for 25 yrs, and as all of us with this dx would love to find answers and rxs for this syndrome
thank you
prema
Hi,
Dr Cheney charges $780 an hour for his time plus about $700 for use of the 3-D echo and the technician. He spends alot of time reviewing your history, explaining your symptoms and why you have them and explaining the treatments. He is like a teacher and wants to educate you. The problem is when you are exhausted and paying so much sometimes you want less education and more of this is what you need to do. Obviously, I would rather understand more, but 2 days of 7 and 4+ hours when you are already foggy is a lot to process.
With regard to the treatments, many of the Rx he uses come from compounding pharmacies and are not cheap and are not covered by medicare or insurance. Although, I am trying to see what I can get covered. As usual, its a battle. There is a post later on that I did for someone about Klonopin where Cheney discusses his front line treatments.
I saw briefly before I couldn’t afford him anymore (and shortly filed for bankruptcy! – best thing financially I ever did by the way.) I just stopped asking question because of his prolixity.
WHY IS DR. CHENEY SUCH A WELL KEPT SECRET???
Actually about 10-15 years ago he used to be the most well-known ME/CFS expert – due mostly to someone who blogged fully about her experiences with him. We actually had far more information on Dr. Cheney’s protocols than anyone else.
Once she stopped he kind of faded into the background. He doesn’t do CFSAC and he doesn’t show up on other opportunities like that. At some point he also dramatically revamped his approach and focused the diastolic dysfunction and the heart. I don’t think many other doctors followed his lead on diastolic dysfunction or stem cells. He appears to be doing that mostly on his own but as you can tell he’s very interested in what other doctors are doing.
I came across Dr Cheney a few years ago on Dr Sarah Myhill’s website. She was very impressed with things that he wrote. Anyone who checks out her site may find a link to things she has quoted from him. I’ve just had a quick look and could not find the document I initially copied, but I did find this summary, if it’s helpful.
http://www.drmyhill.co.uk/wiki/Dr_Cheney_on_heart_function
I have been diagnosed with ME/CFIDS and live in Asheville. I haven’t been to see Dr. Cheney but have known about him since 1986 when they did a TV special on the outbreak that occurred in Nevada. I also led a support group in WNC for many years. I have his CD on “The Heart of the Matter” so know a bit about his theory on what causes CFIDS. He is one of the doctors that first contacted the CDC concerning this illness and at one time was one of two doctors that treated the disease. He has had a heart transplant and doesn’t see as many patients as he used to. I have thought about going to him but haven’t so far because of the up front expense to see him and the expense of follow up treatments. I have a friend who used to go to him who now believes he has Lyme Disease and sees Dr. Jemske in Washington D.C. I hope someday this disease will gain more credibility and get the funding it so deserves. Cort, you did an admirable job explaining Dr. Cheney’s viewpoint and I really appreciate you sharing your journey to get well. I wish you the very best in your quest for treatment and would love to follow your progress with Dr. Cheney.
Thanks – I wish I could take the credit but it was Chris that did the blog. I’m very happy to have it on HR , though.
Dr Cheney’s heart transplant is one of the reasons he started looking into heart issues with CFS. When his heart was failing, he was experiencing similar symptoms to his patients, poor sleep, anxiety, gastro-intestinal issues, brain fog. He found a study by Peckerman (I believe) from the late 90s that equated Cardiac Output to the severity of symptoms experienced by CFS patients. Now, all of his treatments seem to revolve around how it affects the IVRT on the 3D echo.
Yes it was Peckerman. Peckerman is another of kind of sad research stories in ME/CFS. He was consistently finding positive results in the NIH funded Natelson CFS research group. The NIH stopped funding the groups and he never published again.
Hi Becky I will be seeing Dr Cheney for my 2nd visit next week (1/yr is his requirement) and recently moved to Asheville with my mom since I can’t live on my own. Does this WNC support group still exist? I have been looking for something like this as I do not know anyone in Asheville and at the very least could use sme social outlet:) I have been on Cheneys treatments for a year but have not improved. I am 32 and have had this disease for over 12 yrs.
Thanks for taking the time to write up this experience, Chris. This further confirms my current belief that pushing beyond my meager limits is damaging me rather than helping me expand my threshold of energy. I wish this could have been explained to me when I first went to the medical profession and was told “sure, go ahead and exercise all you want.” Years of unnecessary added misery followed with the push/crash cycle.
What does Dr. Cheney feel is the most likely original source/cause of our dysfunctions?
He feels that there is probably some pathogen, viral, or otherwise that starts the ball rolling.
I am so glad a new patient seeing Dr. Cheney will be blogging about him. I have been his patient for seven years now. I went to see him, because I was very non functional for many years with the CFS….and I have improved with his treatments. I am far from well…but I have definitely progressed with his treatments. It is expensive to see him, but I wasted a lot of money over the years not getting anywhere. What I like most about Dr. Cheney is he really does see the big picture of this illness…and he is a very smart man. He has been plugging away trying to see what is going on with CFIDS patients..and he does deal with some of the sicker patients..and he keeps working at it. I was just there May 14th to see him, and he was really working with the echocardiographer to look at my heart, and he is right in there writing down figures and seeing what they mean. I think he is working so much on his research and practice that maybe he is not as visible as he was, but Dr. Cheney is still one of the top CFS doctors…and he knows some stuff because he was in the trenches during the outbreak of CFIDS in Nevada in 1985. He was right there…he has been there since the beginning.
I think everybody is looking to the doctors to pinpoint what “virus” causes CFS as opposed to looking at all of the problems related to CFS. So, all of the limelight is being shown on the “virus hunters.” Meanwhile Cheney is working with other doctors whose specialty is not CFS – Shoemaker (mold), Kane (cell-membrane), Brewer (mycotoxins), but whose patients have similar issues. He is using the successes of these doctors to help treat and improve the health of his patients.
Dr. Cheney was there in Incline Village and he worked with Dr. Peterson and Dr. Lapp for a time as well.
I concur with Lisa. Dr. Cheney is a very bright man with a phd in physics and also an MD. His understanding of this disease is way beyond mine. He has been dedicated to this CFIDS cause since the 1980’s. He has never given up hope and is solely dedicated to helping us. I have improved since going to him last year.
Glad to hear it Joyce. Good luck with Dr. Cheney 🙂
Hi Chris,
Thanks for the blog – it’s very helpful and informative. I would like to echo Greg’s question and I’m curious what supplements Dr. Cheney recommends.
Mimi
Hi Mimi,
See a below reply to GIJs where I was recommending Klonopin. It gives details on Cheney’s first line recommendations. What is interesting is what he does not recommend because it shows a negative response on the 3D echo (CoQ10, fish oil, Vitamin D, A% 5-Methyltetrafolate). I have been taking fish oil, Vitamin D, and CoQ10 for years. I stopped them and have not noticed a difference. I will restart them again just to make sure that they are not having some impact more than emptying out my wallet.
I think I’ve talked to the gal who went to Dr. Cheany on a POTS forum. I don’t think he takes insurance, if I remember right. She didn’t get well from the treatments. I haven’t talked to her in awhile. I think her last attempt with doctors was at Mayo in MN. Not sure how she is these days.
Hope it works well for you Chris. I have diastolic dysfunction too with HyperPOTS. Most of us with this have some pretty bad tachycardia trying to get the blood flow to our hearts and heads. Many of us complain of feeling dehydrated, like the water doesn’t go into our cells properly. And many use meds for diabetes insipidus instead of florinef. Not sure if you’ve had your aldosterone and renin levels checked. Many of us have low levels of these. (I do.) It’s thought that our angiotension II levels are high, but seems this is only checked in research settings. Because, we haven’t been able to get our docs to check us for this. I personally think, if it is high, it must be coming from another area other than the kidneys. (It can also come from the liver and heart.) Because if you study the pathways of kidney function, if both renin and aldosterone are low, angiotension falls in between those two things in the chain of breakdown and if both are low, angiotension should be also. But, according to reports and research, those two things can be low with angiotension high. Some have found Losartan to be of help for this. It also ups your potassium levels. (It didn’t work well for me, despite all “scientific” research made it seem it would have been a good fit.) With POTS they try to increase blood volume in different ways. DDVP and florinef being two things used. But my kidney doc (at Mayo) said ordinarily they would use massive diuretics for low renin and aldoseterone issues. Which we, of course, didn’t do, because of low blood volume. Saline IVs being one treatment used to increase volume, but only a temporary fix. Illness full of twist, turns and paradox. Yet, very complex and interesting.
For sure there is low blood volume and pooling for many of us. Sadly, there are so many subset types of us and what will work for one may not work for someone else. We have found, despite pooling, that compression hose for us with higher bps, it cause it to be higher and also increases our neuropathy in our legs and feet. Many of us have found an abdominal binder to be more helpful and doesn’t seem to hike our bp. The thought is because it cuts down on splanic pooling.
Looking forward to reading your experince.
Issie
Hi Issie, do you also have breathing problems and sometimes panic?
Occasionally now. Not as much as I once did before I started my vegan lifestyle and treatment for a malaria like protozoa.
Issie
Thanks for your insights. In my pre-severe crash years, I kept trying to find a cost effective way to get saline administered, but insurance and doctors were not very helpful. They will give you pills, but trying something benign like saline would not be covered.
and isnt that annoying,
treatments without side effects you must fund yourself
Dr Cheney highly recommends Klonopin which should help with Panic and breathing difficulties, In fact, here is a recent email from him with some details.
Some patients continue their sleep meds and some have tapered some of them off or to lower doses when taking VIP. It is your call to make. However, be aware that a Klonopin or Clonazepam taper can be very problematic in CFS because Klonopin is less a sleep drug and more a redox control drug through the benzodiazepam receptor in the mitochondria (see http://www.ncbi.nlm.nih.gov/pubmed/?term=N.+Brady+RIRR). When tapered, you could experience a large drop in energy and stamina and the resulting mitochondria dependent drop in cardiac output increases adrenergic tone as compensation and this makes sleep impossible. Klonopin has never been a very good sleep drug per se compared to say Ambien or Trazodone or even Doxepin. However, it works well for sleep and even energy at relatively low doses (0.5-1.0 mg) especially when combined with low dose Doxepin Elixir (2-4 drops at 10 mg/cc in water SL, HS). I have not seen significant problems in CFS cases over time (30 years since 1985) using Klonopin as long as it is kept at relatively low doses (equal to or less than 2.0-3.0 mg per day). A few patients are intolerant of Klonopin or have idiosyncratic reactions but this is apparent right from the first dose. If tolerated, it can be taken in a stable fashion for decades and has been reported to protect against Alzheimers, probably via its redox protection properties via the Benzo receptor in the mitochondria and suppression of RIRR seen in low perfusion states like CFS (see above link). This protective effect can be achieved at very low doses (0.5 mg or less) given even in the daytime. I have seen problems of dependency and increasing ineffectiveness as Klonopin doses get up to 4-6 mg per day or more in a few patients. However, the dose for children with temporal lobe seizures is 6-8 mg per day for which Klonopin is FDA approved and the only Benzo approved specifically for children due to its relatively low blood levels at even high doses and reduced addiction potential (as distinct from dependency) due to its long half-life and low peak blood levels.
No one should take drugs if they do not need them for medical reasons and Klonopin is no different but a low energy state with low cardiac output such as CFS will devastate sleep and loss of redox control kills brain cells and Klonopin is strongly indicated in this circumstance, in my opinion, with 30 years of observing Klonopin use in CFS patients. Klonopin along with high dose, injectable hydroxyB-12 (30-60 mg per day) and low dose injectable Magnesium (0.1 cc) with Taurine (0.1 cc) and perhaps Inosine in some patients with serum Uric Acids below 6.0 have been a staple for treating CFS for decades. There is a reason for this success and all these drugs or supplements powerfully affect the redox state whose instability and poor buffering is the core of CFS and a major threat to brain cells, especially from CNS hypo-perfusion due to low cardiac output which is itself due to mitochondrial deficiency as published for CFS by Hollingsworth et al, Shungu et al, Nicholson et al and McLaren-Howard et al.
In the early 1990’s, we were required to taper 30-odd CFS patients off Klonopin for an FDA drug trial (Ampligen). All but two were easily tapered off Klonopin over 30 days with the help of injectable magnesium sulfate despite being on Klonopin for years. However, two patients suffered severe CNS problems (motor neuron deficits in one and psychosis in the other) during the taper and we were forced to put them back on low dose Klonopin where they stabilized. I suspect now that the Klonopin taper caused significant brain injury in these two patients and I have always remembered that experience but did not understand why this happened until the discovery of the Benzo receptor modulated RIRR in mitochondria in 2006 at The Scripps Institute in La Jolla, CA.
On a final note, the generic form of Klonopin is Clonazepam is often much less effective than Klonopin, perhaps because there is up to 30%-40% less active drug in equivalent doses as printed on the generic bottle. More worrisome is that I have begun to see toxic reactions to Clonazepam in the last few years that I have never seen before. I strongly suspect contamination of the Clonazepam by additives that are not controlled and more frequently seen in the poor QC environment of third world pharmaceutical companies where Clonazepam is often manufactured. I think the TEVA brand of Clonazepam is the safest generic but Klonopin is still more effective and safer than Clonazepam. I always recommend starting Klonopin first and then switch to Clonazepam to make sure the Clonazepam is comparable to Klonopin and occasionally switch back to Klonopin to make sure of this over time, especially if you note increased problems on Clonazepam.
So glad some people THINK Dr. Cheney knows his stuff. I think he is Arrogant , and
Has one way of thinking. Had been a patient of his for about 8 years off and on and then went to see him again 2 yr ago as I was having I thought Heart issues. He is not the same Dr. he was years ago. He is Transfixed on the Heart as that is where his
interest is-no where else. Also I found that since I am older he is not as interested in much of anything with me. I cannot afford $10.00 dollars a word in an e-mail.
On the regimen-he put me on as he said I was in Heart Failure I deteriorated to the extreme with Mag shots.
3-Cardiologist have done double testing on me and I am not in Heart Failure.
He also said I had Diabetes Insipedus. I don’t .I could not take shots of Desmopressin. I ask for the oral and he would not let me get an Rx for that.
Told me I was allergic to Oxygen????
What has helped me the most is a CPAP machine that puts out oxygen continuously during the night. Most of my Palpitations have stopped.
I still have bad days and dizziness as feel I have Vestibular problems.
Hope , this saves some patients from wasting alot of money. I too feel it would have been worth it-but I deteriorated from all of his treatments. When any DOCTOR pulls out at book from the 1990,s as Backup- I want to run.
HE IS A GOOD SALESMAN!!!!!!
Carole
Carole
Dr Cheney does not take medicare….but if you have regular insurance that is different, and some patients with regular insurance do get reimbursement from their insurance companies, after they pay up front. They may not get full reimbursement. I am on medicare so I sign a waiver and pay up front. Issie…found your comments interesting on POTS….and I am looking forward to hearing Chris’s experiences with Dr. Cheney. My tachycardia has improved a lot with the treatments dr. cheney is doing…but I don’t want to blab about the treatments since Chris will be blogging soon about them.
Thanks so much for sharing this. I think Cheney is tops, and has been since 2009. It seems he hasn’t changed his theory in five years so that charge that he is constantly doing so doesn’t stand any longer, and he’s created some ingenious ways of demonstrating his thought. He’s a genius. Please continue to keep us posted on every word that comes out of his mouth.
I agree, Graeme. Dr Cheney is tops, his thorough well-based explanation makes perfect sense to me. I’m sure I’ve got all of that.
The nearest I’ve got to his tests is an ordinary echo which indicated low blood volume. Even if his test was used for diagnosis only it could never again be said that we have ‘medically unexplained symptoms’!
One of the nice things about being a Cheney patient is that he is frequently sending emails to keep you in the loop. He is frequently updating his information and recommendations as he gathers more knowledge for his patients and other doctors. This would be another reason to justify his fees. He answers questions by email pretty quickly and unless there is a specific complication that requires a significant amount of his time, there is no charge. Other than my current Primary Care doctor, its a rare thing to get this type of added attention and my PC doctor is getting worse about responding.
Chris is sending me Cheney’s emails on various subjects. I must his willingness to share is impressive and very unusual. I wish more doctors did it.
Thant sounds great in theory -but no other Dr. would accept his Echo
when they could find a machine to run it or any of his tests.
Carole
Les Simpson, (Ph.D in hemorheology) has done years of careful research into the role of red blood cells in chronic illnesses, including ME, and spent several years going to ME conferences and visiting support groups, and housebound patients – in the U.S., Canada, the UK, Australia and New Zealand. Hemorheology is the study of the physical properties of blood. It is not taught in medical schools, and research is mostly ignored. I don’t understand why his ideas have not been included in the canon of theoretical and practical thinking about ME/CFS. It seems to me to make sense, and to provide an additional layer of explanation for lots of the other research findings. It also points to simple and relatively inexpensive things that we can try out, to add to all the other things we are trying.
So here goes: Every cell in our body depends, for its normal functioning, on the red blood cells performing their normal functions, which are to deliver oxygen to the cell, and remove the waste products of normal metabolism. Many areas of our body depend on the system of tiny blood vessels, the capillaries, and the ability of our red blood cells to pass through these capillaries to reach the cells they serve. Capillaries can get as narrow as .5 mm in diameter. Red blood cells have a diameter of about 1.5 mm, but in the most usually occurring shape – a biconcave discocyte – a flat, round shape with a hollow on each side – they can curl up (deform) and become able to pass through these tiny blood vessels. Medical students are taught that all red blood cells (erythrocytes) have this shape. However, micrographs of immediately-fixed blood samples show that even in the blood of healthy individuals, there are a range of other shapes which occur – Les has identified six categories – cup forms, forms with irregular edges, etc. These ones are not able to deform enough to get through the capillaries. In chronic illnesses, his immediately-fixed samples show that there is a much higher proportion of these irregularly-shaped, non-deformable cells in the blood, which means that capillaries may be blocked, and the supply of oxygen and removal of waste products is much reduced. Our muscles, cognitive areas of the brain, and the endocrine system, are extremely vulnerable to these effects. To me, this seems a simple and uncomplicated explanation of how our symptoms arise. Les does not claim to know the original cause of these changes in the red blood cell population, and he does not offer a cure. However, he does say that 6g of fish oil per day, or 4g of genuine EPO per day, or Vitamin B12 as hydroxocobalamin (not cyanocobalamin), or pentoxyfilline, are each things which can improve blood flow. Each may help a proportion of ME sufferers, and he does not know why there is a variation, or why some people with ME do not respond.
He has spoken with many of the old hands in the ME world, and I really do not understand why his ideas have not been taken up. It seems that sometimes scientists are more interested in discounting than exploring ideas other than their own. When someone reported that EPO wasn’t helpful, Les discovered that only a few of many products on the market described as EPO were genuine. When other research didn’t confirm his results, it turned out that the samples were treated in the usual way – washed in saline solution and left for a while. Samples treated in this way allow the red blood cells to resume the usual biconcave discocyte shape. Only if the samples are immediately fixed (a process used in operating theatres) will the irregular shapes show up. Les is very clear about this, and research which does not follow the protocol he describes will not get the results he reports. Scientists testing the validity of reported research should be careful to be using the procedures described in the research they are attempting to duplicate.
I suggest that it is worth any ME sufferer’s time/money to try out one or another of Les’s suggestions for a few weeks. I note that B12 is one of Cheney’s recommendations, and the Canadian Guidelines do at least concede that there is ‘anecdotal’ evidence for the usefulness of fish oil. Les’s 120 papers and two books do not constitute ‘anecdotal evidence’, but there you go!
Very interesting, thank you for this Nancy!
In the early 1990’s while doing his research, Doctor Simpson visited my Canadian city to collect and “fix” blood samples from ME patients. A few months later, I received a detailed report including a micrograph (photo) of my blood cell sample. My noteworthy results were as follows, with figures in parentheses indicating averages for a woman:
Normal: 6.9% (28%)
Flat: 80.3% (43.6%)
In my case, Doctor Simpson’s report indicated that the large percentage of flat cells would have “an adverse effect on capillary blood flow”. It also mentioned, however, that cell percentages should not be compared with the results of others as the effects of cell shape relate only to the vascular system from which the cells were obtained.
Thanks for bringing this to our attention, Nancy. Presumably, Les’ papers were mostly published after I submitted my blood sample. Definitely another avenue for me to consider.
The reason they are not included as everyone with CFIDS does not have the same thing.
And is not treated the same way.
18 months back I said ‘it’s in my blood, the probem is in my blood’
then eventually Live Blood Analysis demonstrated exactly these problems. The B12 H lozenges were like feeding me oxygen 🙂
According to DR Dennis Courtny MD, fish oil prevents red cell aggregation (clumping) that could cause a stroke or heart attack! Is this a big deal? I have relied on fish oil for the past ten years primarily for that reason. RP
There is one problem with fish oil however, Dr. Cheney says it oxidizes easily, and that can cause issues in the body since our cell membranes have been hurt by oxidative stress. He recommended that I eat fish when I craved it but not to overdo on the fish oil. He likes colavita olive oil because it has a lot of bioflavonoids in it to prevent the 3’s and 6’s from being oxidized. I have a hypercoagulation disorder…but find the fish oil a bit too strong for me.
Lisa Schicht
Because I was diagnosed with POTS from him- have had it. He put me on High salt water content alkaline water. To Drink. My Blood pressure shot up- normally low and I became very sick.
Nice to read feedback re Les Simpson’s information. These are just suggestions and it’s good not to be dogmatic, and be aware that we are all different and may not respond to the same things. It’s just good to know what people find helpful.
The bee in my bonnet is that it seems that if we conserve muscular exertion enough, our body seems able to find a way for us to improve, and until we have some definite drug treatments, or alongside the treatments we are trying out, doing aggressive resting seems to me to be a good plan. I strongly recommend adopting a lifestyle planned around continuing normal life as much as possible while using every possible strategy/aid that will allow us to conserve muscular exertion – so that we can do the essential things, and some of the fun things, and still leave our body systems enough energy to do what they can to help us get better. Until we had antibiotics and fancy symptom-relief, over the counter drugs, and the culture decided that physical exercise was good for everything from cancer to warts, the idea was that when you got sick, you went to bed and stayed there until you got better. Now resting seems to be regarded as a positive danger. But as we continually find out, for us it is exertion that can be the positive danger. In fact I suspect that the modern pressure to just take the tablets and carry on (all those adverts for pain relief, etc) is probably why instead of getting fully over viral infections, we get ME. We just don’t give our bodies the chance to get properly over things.
Something that makes a significant difference is keeping our head supported – it’s pretty heavy, but we are usually unaware of the amount of exertion needed to hold it up. Just that one habit, of always finding a way to lean back and support your head (highbacked chairs in a restaurant, office, or your home, recliners, driving with the back of the seat on a slant instead of upright, etc) can make a big difference. Being able to keep track of what is going on in a classroom or meeting; being able to enjoy a social outing instead of losing the plot and getting exhausted…all this stuff doesn’t require a prescription, a visit to a doctor’s office, or cost money….
I think in the US especially, but all over the world, big pharma has got us well trained to think that cures come in the form of pills, and we can use up a lot of energy trying to find the right pills.
Having said that, I do find Les’ suggestions helpful (if not fish oil, then EPO?), and also that CQ10 (currently, one 120mg per day) makes a huge difference.
You guys are miles ahead on the technical stuff – I’ll be looking forward to how Cort’s treatments work out. But…$20,000 ….. how many of us have that kind of money? It’s scary what people have to give up to get treatment.
Hi Nancy,
Regarding the “bee in your bonnet”, a few years ago I experienced the value of what you describe as conserving muscular energy, and aggressive resting. While experiencing worse-than-usual cardiac symptoms, an unfamiliar doctor sent me to ER with a letter indicating I must be seen immediately. This occurred the day before a long weekend, and with a reduced staff to perform the required tests, I was admitted. So, I had four days of enforced bed rest prior to my treadmill test. No cardiac abnormalities were detected, and I experienced no PEM afterwards. For several days after leaving the hospital, I felt considerably better than usual, and commented that I wished a lifestyle requiring no food prep, or household tasks, was possible. In contrast, it took days to recover from a previous treadmill test done with no prior rest period.
Yes, aggressive rest works — at least for me. The challenge is determining how to do this while still managing the non-discretionary requirements of daily life, and having a bit of fun at the same time.
Aggressive rest – I like that name for it!
When I can afford it I go on holiday on a cruise ship. Karen, for me that provides the break from cooking and cleaning and all the oddments of everyday life that take up so much more energy than we realise.
Confession, though – instead of aggressive resting I put the energy into ballroom dancing at night. I don’t mind doing nothing all through the day as long as I can dance the night away! (As there are not enough Gentleman Dance Hosts for all the single ladies, I don’t push myself too far with the dancing, but just enough to enjoy myself and feel alive again.)
TRUST ME-I DON’T KNOW WHERE YOU IVE-BUT YOU CAN FIND TREATMENT FOR LESS THAN $20,000.00 AND A BETTER DR.
Thank you for your thoughtful and in-depth responses, Nancy. I’ve thought about that too, that the rise of antibiotics–a great advance in medicine in so many ways to be sure!–shifted the expectation of medicine from one where concoctions aided the rest-recovery process to one where concoctions are the recovery process. In history and literature we accept that people in the past gave the body time to recover, that it could take weeks or months, as well as that “they were never the same after” a particular illness. Of course I don’t want to stay in the “never the same after” camp where I’ve been for a decade or more, yet it seems that the societal expectation that we SHOULD BE better is the part that’s ill-advised. Well, of course we have the perspective and time to get philosophical. Sometimes that sense is a helpful respite though from maintaining the level of dissatisfaction necessary to push for change.
Follow.
Following thx
not just heart,but heart,brain,kidney–all have problem of microcirculations.
pm2.5–air pollution have great impact on the CFS/ME.
look up in PUBMED OF PM.2.5–we can understand most of our symptoms.
mono,giardia–all result from immune suppression from toxic environments– pesticide,
air pollution(diesel exhaust gas)
“Long-term Air Pollution Exposure Is Associated with
Neuroinflammation, an Altered Innate Immune Response,
Disruption of the Blood-Brain Barrier, Ultrafine
Particulate Deposition, and Accumulation of Amyloid β-42
and α-Synuclein in Children and Young Adults”
look up this article
this new finding will help you
TAE PARK,M.D.
The date of my onset of symptoms was almost exactly like Chris. Mono, Eptein Barr and CMV. Also Pesticide exposure and I worked in a dental office.
My saving grace at the time was an Infections Disease Dr. that was exploring options for Epstein Barr and also Aids. Finally went exclusively with Aids.
He started me on a double blind study of Immune Globulin made at the time by Bayer.
My improvement in 3 weeks was dramatic with Immune Globulin shots.
I was doing well on this regimen and a strict diet-until Bayer sold out to Telecris and the product went generic and a detergent was added. I started having dizziness and
Cognitive problems from this change alone. I also could not handle any stress.
Then came the heart issues-that is why I went back to Cheney. Heard he was into Heart issues now- as he had not changed my regimen before so I did not need to see him again.
My thoughts now are when I told Cheney’s office I was too sick to go back to Asheville just for an Echo , (which is all he did to me before ) and talk, talk, talk.!!!!
They told me he was very strict on his patients coming back within a year. I suggested a phone conference instead to see if we could tweak things to see if an improvement was possible.
The phone conference would have been $750.00. I declined.
I am now seeing an Environmental Dr. here where I live and she is up on most of the things he is. Is very conservative and very careful. Also knows him well.
She e-mails me back answers to any questions and will see me any time. No charge for e-mails. Does Vitamin IV’s and also has me on Hormones compounded (low doses).
Chris- since you are young and going to advertise his comments-you may get better care. He loves the spotlight and no one is saying he is not bright. But he has to prove he is right!!!!!
However I still say you can do better with your money.
Will follow with interest.
Carole
Hi Carole,
I am sorry that you had a bad experience with Dr Cheney. I can understand how he can come across as arrogant. It is a a trait I have noticed in brilliant people as they tend to dismiss other’s opinions. The concept of “suffering fools” whether the people are fools are not. They don’t have the patience.
With regard with Cheney being to uber-focused on the heart, I agree. However, he is looking at other issues like mycotoxins and cell membrane injury. He is working on ways to improve cell membranes and improve the detoxification process which is a definite issue with CFS patients. He is still using the IVRT to asses whether these treatments are effective or not.
As with all doctors, you have to realize that he is a person with a specific area of expertise and noone really knows how to actually fix ME/CFS. Its still up to you to take his advice and decide on how or whether to apply it to you. I have called myself a “science experiment for years” as I am constantly trying new ways to improve my health. He is giving me new things to try that my other doctors have not. My health has improved somewhat since I started following some of his protocols. Nevertheless, I have not yet found a magic bullet from him that causes me to reach a new level of capability. Its slow and steady progress, and yet, I still have more treatments to add from his aresenal. I am trying to take it slow and evaluate what works, both from a cost perspective and a need perspective. Why pay $400 a month for 60mg of HB12 daily when 10HB12 leaves me feeling the same.
So, I continue being the guinea pig in hopes that one day I can say I feel normal (at least most of the time).
Chris- His specific area of expertise is MONEY. He did not offer to do any blood test on me-just an ECHO. And basically said-
“Be careful walking to the car”. I had walked 2 miles before I went in to see him that day.
My friend that went with me to his office said-“Well I guess he didn’t do any blood tests because you are dying”. We laughed believe it or not for at least an hour off and on.
BE CAUTIOUS AND CAREFUL!!!
Carole
I have to disagree that Cheney’s expertise is money Carole! Yes, his fees are high and that can be really upsetting but he’s also devoted his career to this disorder and he’s always looking! He’s very creative – he’s talking to other doctors. I think he’s very focused on ME/CFS and that’s a good thing.
We won’t know if anybody is right or wrong until this thing gets figured out and we can say Oh – Dr. Peterson had a piece of the puzzle and Dr. Cheney got this slice right. ..So much of it isexperimentation at this point.
Cort- Not saying he is not interested in the research or the
the process. But the financial part keeps many people from even being able to consult with him.
Isn’t that why you quit seeing him?
That is not why I did not go back. His only interest to me was money. He is smart, he is brilliant. Doesn’t matter if the people that need his expertise can’t get to him.
I do not agree he is contributing at all. I know of none of his patients that are alot better or cured.
He has a lot of Theories. I know a lot of people that have seen him and then left his practice.
I hope Chris has a good outcome- but most of the Physicians in CFIDS do not agree with him.
Like I said before- There are some very good Infectious Disease dr out there that can help us. Try them. Also I would definitely rec that anyone with Dizziness or OI see a Neurologist and have a Brain MRI. This was never mentioned by Cheney.
Carole
Carole
Thank you for being that guinea pig, Chris. The experience of you and other patients who are able to get to these boutique physician experts and then blog about it is a tremendous help to me. I am able to see how my symptoms and tests over lap or not, print out the protocols, take them to my doctors and see if I can try them without the financial expense and the PEM payback. I see this as a way privately funding research that sometimes has been they only way things are moving forward. You and others like you may be going into debt, your extended family may be helping (which brings emotional debts that may have baggage as well), and you are trying new treatments knowing that you may have a poor response that can set you back as well. This is a sorry state of science and medicine that the situation exists like this, but under the circumstances that it does, thank you for your courage and willingness to do all that.
And Carole, too, thank you for your perspective and sharing your experience. It is an awful lot of money and effort for people to see specialists like that, and I’m sure your counsel has helped others make a decision to not try that route.
I’m in the middle. I was on a waiting list for both Cheney and Petersen for a couple of years, and when their offices contacted me I did not feel that I could follow through because of the expense. But I also had been sick longer by that time and the resources of information like this became more available, gave me better tools for measuring my experience against others and understanding how ME/CFS presents in me. I “train” all of my doctors in ME/CFS science by giving each new one the IACFSME primer on a first visit and printing relevant abstracts for each follow up, and as a result I really do think that I get good care and feedback from my GP as well as my specialist, Dr. Chia (who accepts my HMO and is just a couple of miles away). Dr. Chia has no doubt paved the way in my neighborhood for doctors to be more open, but I play an important role in expanding their knowledge by bringing in blog entries like Chris and abstracts from studies like the ones Dr. Park suggests, which I’ll read next.
We all need each other. I’m sorry you’re all on this path, but I’m so grateful that you share your experience.
Hi Carollynn,
Thanks for that very thoughtful and insightful commentary. You have hit the nail on the head. If my experiences can help others without having to go through the expense then I feel it helps some of my financial as well as emotional costs associated with this illness. The more we can communicate and share, the better chance all of us have on finding something that may help us.
DR.CHENEY’S interest in heart is probably from his personal experience.
Namely “CARDIOMYOPATHY”
The heart muscle is greatly weakened by poor microcirculation and myocarditis
which is from TNF-ALFA,IL-1,IL-6
THESE CYTOKINE is very much increased in CFS/ME patients.
Chris,
I’m also interested in going to see Dr. Cheney. Does he do any invasive testing like, say, spinal taps?
Hi Kristi,
He just does the 3D echo and a some blood work and takes a detailed history of your condition.
Chris
Hi Chris,
I just wanted to know other than klonopin what the treatments from Dr.Cheney are?
Thanks, Tim
Hi Tim,
I will be blogging about these treatments in more detail. Cheney is always tweaking his current protocols. Here are his first round recommendations. From Cheney…
In my opinion, with 30 years of observing Klonopin use in CFS patients. Klonopin along with high dose, injectable hydroxyB-12 (30-60 mg per day) and low dose injectable Magnesium (0.1 cc) with Taurine (0.1 cc) and perhaps Inosine in some patients with serum Uric Acids below 6.0 have been a staple for treating CFS for decades. There is a reason for this success and all these drugs or supplements powerfully affect the redox state whose instability and poor buffering is the core of CFS and a major threat to brain cells.
Low dose VIP (< 1/10 cc SL) quickly raises cerebral output and/or cardiac output which may be critical to proper CNS function and also reduces inflammation via T-Reg VIP receptors, especially over time. VIP also induces hepato-biliary function and improves gut motility which is critical to detoxification, especially in those with very low plasma VIP which is true for 98% of CFS cases.
Kirkman's Colostrum at 1-2 Tbsp per day "in the free". Unpasturized Colostrum contains Gc protein which helps regulate Antigen Processing Cells or APC cells and one of the best anti-inflammatories I know of, even better that NF Kappa B inhibitors or NSAIDS which are way downstream from APC's.
Finally, I would use Liquid Mineral Therapy (LMT) by BodyBio to balance key minerals which will help detoxification enzyme function and helps eliminate heavy metals.
Interesting that you should mention the Colostrum- I got sicker on that and Cheney said it was because the COWS had eaten grass with Pesticides in it???
(They changed my form of Immune Globulin so I was trying the Colostrum instead.)
Craziest explanation I have ever heard. Took exactly the one he rec and it was injectable..
Wish you nothing but the best Chris- Just don’t expect too much.
Carole
Thanks Carole,
Conceptually, the colostrum could be making your immune system kick in which could mean that there are possible herx reactions. Cows eating pesticide laden grass is definitely over-reaching for an explanation of your reaction. I tend to be a skeptic by nature and I could definitely offer some potential conspiracy theories for Cheney and his actions. So, I continue to keep my skepticism high, but at the same time try to analyze his recommendations.
Hate to even go here but some of you need to ck the companies Cheney rec as some are Pyramid associations. Whether he is one of the beneficiaries , I don’t know.
Please, Please be very careful with some of the recommendation from him. No one wants to believe it is all about money. I was one of them. Please just consider the fact- he has lost his place in line and is to me DESPERATE.
OK it is MONEY AND EGO!!!!!
Carole
A cautionary tale —
My son went to Dr. Cheney in about 2007-2009 at the age of 42. He had had ME since 1991 and had been to various doctors. One was particularly helpful but left his practice in the early 2000’s. Other doctors had not been as helpful, and Eric thought Dr. Cheney could really help him, knowing of C’s reputation. Eric was very sick, and his father had to drive him to Asheville for each visit, from New Jersey, as Eric could not have driven himself.
Eric had about four three-day sessions with C over the course of his treatments. Cheney was promoting at the time new treatments which he sometimes described as “just food” and other times as being nearly stem-cell powerful (the same treatments). The drugs were formulated for Cheney. They were not FDA approved. Eric took all the medicines that C. prescribed or recommended if they were not prescription drugs. This new crop of concoctions of Cheney’s made Eric much worse. All his symptoms were exacerbated. Consultations with Cheney did not result in any helpful antidotes. The best Cheney seemed to be able to do was advise Eric to start on what turned out to be a cockamamie diet and test that went with it which was very expensive – $1000. (Alcat Diet – Google this; see 2010 report from S. Africa) This was worthless and did not help a bit.
Cheney also ratcheted up Eric’s Klonopin and Neurontin prescriptions to the maximum levels (and possibly even over the legal limit) to try to cope with Eric’s severe symptoms. Nothing worked. Eric called Cheney numerous times between visits (very costly per minute), but Cheney had nothing to offer which would undo the harm he had done by recommending his experimental drugs/treatments. Eric felt he had been left to drift in a sea of pain, and Cheney did not care at all. Cheney never followed up on his own volition to call and see how Eric was doing. Eric and his father, who had been present at all the visits, concluded that to Cheney Eric and other patients were nothing but lab rats (with money).
Our primary care doctor believed that Cheney was guilty of malpractice. The only reason that we did not report Cheney to the FDA for using these treatments on his patients was that we did not want to add to the chill in the medical profession that has always been present regarding CFS. I know of doctors – some very fine ones – who specialized in CFS who were driven out of the profession or out of the specialty of CFS by others in the medical community. We know there is a significant bias against the disease (largely because of its name), and it is very hard to get doctors to learn about it and treat patients.
Btw, those treatments that you are being prescribed, Chris, Eric also had – nothing new in them, as you say. Cheney has nothing new to offer that is effective and safe. But he does charge a lot to do the voodoo that he does so profitably.
Eric never did recover to even a pre-Cheney level of sickness. He died June 1, 2014. In our opinion, Cheney was a partial cause of his death.
Hi Billie,
I am deeply saddened for your loss. Having come through the year I had last year, I am blessed to be doing as well as I am. I, too, had to have my brother-in-law help drive me up for my visits. I agree with your sentiment that we (myself included) are lab rats for these doctors. I have always tried to make myself a person to the doctors, but without regular contact and without the right doctor, I will continue to be specimen 239. I don’t think Cheney or any of the other doctors intend to do harm, but with this condition which has no answers, desperation sets in. There have been other doctors who could also be labeled guilty of malpractice in the deaths of other CFS patients. Having spent countless hours looking for answers, I know that many people are willing to try just about anything – many things I find far to scary to consider.
I have emailed Cheney about various treatments I am thinking about and for the most he has warned me against most of them. However, it is only his advice and if I think something might have a benefit and it seems that the potential for negative reactions or setbacks is low, I may chose to ignore his advice and try it myself. I tend to try and take things slowly, but I do have a healthy fear that any of these treatments might make me worse.
With regard to Cheney having no new treatments that are effective or safe, the treatments I mentioned earlier are only a subset of what he is working on now. Also, so far except for a few bad days when I started one of the treatments, I feel like I am improving. I, also, believe its possible that it has nothing to do with Cheney and his treatments. My plan is try his suggestions and as long as nothing has a significant negative impact stay on them for the next 6 months. At that point, I will re-evaluate based on whether there have been continued positive results or I remain at this level. In the meantime, I continue working with other doctors and look for other answers.
I guess I should relate my experience with Dr. Cheney – it was relatively brief – about a year and a half. Finally I had some money (briefly) and I immediately booked over there.
For the most part I don’t remember it going particularly well. I tend like everyone else to remember the negative stuff. One incident was kind of laughable – they inputted my weight into the exercise machine as kilograms not pounds – throwing the results way off. I caught it (not them) about a month later. That was just one of those weird glitches, though – not typical at all.
Cheney was very prolix which was a problem because he was so darn expensive. He identified my mercury problems (that was good). I got angry when he had me do some expensive genetic tests that didn’t seem to lead to any treatments and we almost split at that point. His office manager was like a bulldog – demanding payments in a very aggressive manner. It was pretty clear on one visit (after flying across the country) that he had not looked at my file beforehand. That was really upsetting
On the other hand he was good at answering emails and he’s now really good at sending out emails telling patients his thoughts on treatments. I felt he was pretty compassionate and I wasn’t able to stick with him long enough I don’t think. What I really like about him is that he is always investigating, always talking to other doctors. I don’t if he’s right or wrong but he’s definitely someone to keep an eye on.
I second Cort’s opinion, except about being compassionate.
I wrote a ‘blog’ after my visit stating basically that you don’t always get everything you want in a practitioner. The bottom line with Dr Cheney and with every practitioner is how effective they are. It’ll be interesting to see how Chris does – I hope it goes well.
I too have never recovered from my last treatments from him. I was walking on a treadmill 45 min a day. I was having Heart Palpitations at night. CPAP machine took care of that.I do not have the energy to walk on the treadmill anymore.
I did not take the Gabepentin, or Klonopin as I was not in any pain and felt even though I had dizziness I was still able to function.
I am not back to my Pre Cheney state.
Why I ask will no one sue this man.? I am suing a Vet at the moment for the death of my dog. He has been sanctioned and is retiring.
The reason is WE ARE DESPERATE!!!!!!
I wrote this before and I will write it again- I had a dear friend about 20 years ago that was a patient of Cheneys commit suicide. She was on Kutapressin. Her husband lost his job and she could not afford the injections.Not Cheney’s fault- but he knew of her suicide and never contacted anyone in the family.
Infectious disease Dr. are an alternative to Dr. like him . Also I am seeing an environmental Dr. here that is treating me. Her first line of defense is no
INVASIVE PROCEDURES – MEDICINES OR DETOX UNDER ANY CIRCUMSTANCES.
I am so sad for your son’s death. I know how I hurt for my friend Donna-who had just had her first Grandchild.. She took an overdose of drugs. Please people- know- He does not care-You don’t pay his fees -you are gone!!!!!!!!
My deepest sympathies.
Carole
Sadly, Carole does speak the truth – people- know- He does not care-You don’t pay his fees -you are gone!!!!!!!!
Eric’s death date was 6/1/11, not 6/1/14. Mental typo.
Billie, you wrote:
>>>Eric and his father, who had been present at all the visits, concluded that to Cheney Eric and other patients were nothing but lab rats (with money). >>>
One wonders, if it is true that Cheney’s patients are lab rats with money, how valid his “research” is. Even Dr. Byron Hyde has said that wealthier patients have a “cushion” to fall back on…which I assume is better health care, more home help, etc. It doesn’t seem like to me you would be comparing apples to apples if you mainly researched only people who could financially afford to see you…and weren’t researching people who couldn’t afford your fees.
I’m sure Cheney uses phrases like “in my practice, I see….” to cover his @ss. And it may be true that “in his practice, he sees….” yadda, yadda, yadda. But not everybody with this disease can afford to see him “in his practice.” So I have to wonder how valid his “research” is.
Sorry- Forgot to mention in my other post. I ask Cheney this last time when I saw him if he would consult with my Primary Care Physician -He said “No- I am not going to teach other Dr. what I know”!!!!
This to me is the most “Arrogant ” statement I have ever heard.
Just a last footnote.
Chris- interested to hear what you think later!!
Carole
Thank you, all, for your condolences.
To speak to Sue’s point about whether Cheney is a researcher. He is not, no matter what he says. He is only impersonating a researcher. This was one of the things that made us so mad. If he were a true researcher, he would naturally want to follow up with his patients that he used in his research (supposedly all of his patients would fit this category). He never initiated a call that was not planned for in advance by Eric and that wasn’t billed for. Once Eric stopped calling him, that was it – no follow up whatsoever. Eric could have died two months later or two years later – Cheney did not know or care. Since Cheney was using new treatments that he had designed, wouldn’t you expect that a serious, sincere, honest researcher would want to know how this patient was doing, particularly after knowing that Eric was having such a difficult time?
Eric and his father never, from the first visit, thought that Cheney cared about Eric but rather did view him as a lab rat. (They did not come to this conclusion after the bad results). He talks incessantly (I have tapes of the visits), much about himself and his theories, all the time running up the bill. Verbose doesn’t begin to describe this aspect of Cheney. And his theories are so elaborate, so technical that a lay person would have a very hard time determining which of his statements are incorrect.
Chris, good luck. Maybe you will see benefit from your visits. However, as an experiment – try questioning him on what he is treating you with and why this is so much better than other ME/CFS specialists’ treatments that do not cost nearly as much. I bet you will get an elaborate gobbledegook answer that you do not understand and some huffiness that you would dare to question the “master.”
One other thing is One of my Cardiologists said the Echo machine he used was so old and out of date, that he had to have his Tech go next door to another clinic to view it.
This was about 2 yrs ago.
He told me dead out “He is incorrect”. I had a Heart Cath and I have a relaxed muscle that is working and a small amount of blockage 20%. I am on no Heart meds.
Also had a Calcium score test by this Cardiologist.
Please rethink that we have to see a Chronic Fatigue Specialist to get better. Environmental and I have found Infectious Disease are on top of things also.
And don’t expect you to go bankrupt to see them.
Carole
Do you know how Eric passed away?
I seem to be reading that people due pass from this disease and that really scares me. I currently have severe cfs and am bedbound
Andy- Hate to say this but alot of the Cfids patients commit suicide.
I have known several. When someone tells you unless you pay gross amounts of money or you are not going to get better-if you believe them-
They give up. They are too weak to fight anymore.
Shame on all of the Physicians that do not take Insurance and charge elaborate fees.
The ones that are going out of the country are just as ridiculous as using Dr. Cheney. They are laid up for weeks or months after the trip.
I know none that are alot better or cured!!!!
Anyway- Chris Let everyone know
Carole
Andy, I am very, very sorry you are bedbound. Eric committed suicide after having ME for 20 years because he could not stand the pain he was in from so many places on his body and saw no hope for any treatments coming along that would help him. He did not expect to get all better, but he did want to function and think better. That was in 2011. There are more treatments being used off label now – rituximab and the antivirals primarily. If Ampligen could get approved, it would help many, many patients and be paid for by insurance and stimulate other pharmas to invest in the disease (watch CO-CURE for a request for letters to be sent to Congresspeople and the FDA for a Congressional hearing about this). I hope you have a kind doctor at least. Eric early on found that evening primrose oil gave him a good deal more energy. If you haven’t tried that, it might help; it won’t hurt.
Billie -I am so very sorry about your Son. One of the things that helps me the most is Hydroxy B-12 sub q injections compounded and then IM 2 times weekly.
This and no sugar and a Gluten free diet. Which I was on when I went to Cheney.
I am also on a liquid vitamin supplement from Mother Earth mixed (small amount) in water and hormones from Environmental Dr.
Again- I can feel your grief in your writings and I hope in some way just expressing your feelings will give you some peace.
Also some of the coping strategies from the Dr. at Stanford were a lot of help.
Cort- i want to thank you for your courage in expressing your feelings. We all need to just tell the truth about how we feel about whoever.
No one is judging anyone.
Carole
I contacted Dr Cheneys office years ago in a crisis in the early years after diagnosis
I was told they did not take medicare and when I realized what the cost were to see him
I was not able to go.
They knew it was urgent and that I had no support system from my
internist nor my family and it was urgent that I see someone who was kind and understanding..
so no big money to hand them..and no one cared to see me to save a human being..
I am here by the grace of God and Jesus Christ today and I have to say there are all kinds of
stages with this disease..
Mine started with a flu like virus, bronchitis often the next 3 years,
gastro infections and acid reflux , depression, anxiety, sweating episodes, low blood pressure
feeling faint , not able to stand long without leaning on a door or something, headaches,
irritated bladder and pelvic, stinging in arms and legs, pain all over from head to toe,
multiple chemical sensitivity illness, blurred vision..and almost all of it today 30 years later.
I have no one but an internist that I see once a year..I do not take the drugs they recommend
I am no longer on antidepresants, I take vitamin d 3 6000 units a day , flax seed oil . magnesium
capsules , a daily vitamin and that is all..an occassional Clonzapam, occasional percocet with zofran and that is it..
Learning on my own that the bladder pain was not anything but fibromyalgia pain after painful
cystoscopes and hospital visits, learning that gastro was over growth of bad bacteria and changing and getting off bread, pasta, sugar and most white carbs..has helped me.
Learning on my own that cfs waxes and wanes for me….
and just learning to try to not beat myself up as I have done for decades…
because my mind wants to stay physically busy and I just can not do it often..and when I do I plan to be down about a week in pain and exhaustion..
I do it some times anyway..knowing what will happen..
I have determination…and some joy and happiness in that I try to do for others at a nursing home or on line ..send cards to cheer others and take my mind off myself..
and I usually always pull back up and feel that joy….. due to my faith in Jesus Christ.
Sheri
Hang in there Sheri! Good luck with everything…
Well done to Chris and to Cort for their work in bringing this to our attention. There is a sense here of patients going around in circles for years, getting nowhere, losing hope and losing money.
Dr. Cheney has been effective for some patients and not for others. This being the result of an illness which contains several subgroups which complicate s the diagnostics and the treatments. And the fact that most doctors, including Dr. Cheney, do not carry all of the required tests to identify the known biological abnormalities, dysfunctions and infections present in a patient and subgroup. A complex illness such as ME/CFS requires a high level of diagnostics and dedication from doctor and patient.
The only proper and meaningful work for an ME / CFS doctor to do is to carry out all the tests, identify all the biological abnormalities and dysfunctions and infections and then treat them. A proposal for this is at http://www.me-ireland.com/structure.htm#8 . Otherwise, patients will continue going around in circles for years, getting nowhere, losing hope and losing money.
There is a need for all doctors to train each other and receive expert training in ME and CFS treatment and engage in constructive dialogue about research and new innovations, and this too is presented here at http://www.me-ireland.com/training.htm
The work of Les Simpson and red blood cell structure is relevant and has been integrated into ME and CFS clinic proposals and diagnostics http://www.ireland.com/structure.htm#m
Cort,
The info re Dr.Les Simpson was fasinating, and I remember reading about him and his blood work in Oslers Web by Hillary Johnson.
Can you or anyone else point to any further sources of info, or any other avenue to obtain more info regarding his prolific and very relevant work?
Thanks,
Megin
http://www.ireland.com/structure.htm#m
Hi David,
The link does not open. Do you have any other sources?
Thanks,
Megin