



Let’s put aside questions of whether a disease is going to kill you or not and concentrate on what happens if it doesn’t kill you. Let’s say God said you had to have a chronic illness but he/she would allow you to choose which one to have. On what basis would you make that choice? My guess is that most people would pick the disease that allows them the highest quality of life and the most functionality.

If a disease doesn’t affect quality of life – how much does it need to be addressed? If it does significantly affect QOL – how much more urgently should it be?
A disease that doesn’t impact our ability to function or to be productive in society or our quality of life, may be a disease that doesn’t need a lot of attention. A disease on the other hand, that significantly restricts our functioning is a disease that our society, purely from a pragmatic viewpoint, should pay a great deal of attention to. A disease that significantly impacts our quality of life is a disease that we as human beings would dread, most of all, of having.
People with ME/CFS often assert their disease is not taken seriously enough at their doctors office, by the public, by their families or by the federal government.
A Danish research group put the impact of chronic fatigue syndrome to the test recently. They compared the quality of life scores of people with ME/CFS with people who had serious medical disorders.
It was put up or shut up time. For ME/CFS to be considered a serious disease it had to pull its weight against diseases like multiple sclerosis, cancer, rheumatoid arthritis and stroke. Could it?
Let’s find out.
The Study
The Health-Related Quality of Life for Patients with Myalgic Encephalomyelitis / Chronic Fatigue Syndrome (ME/CFS) Michael Falk Hvidberg,1,* Louise Schouborg Brinth,#2 Anne V. Olesen,#1 Karin D. Petersen,#1 andLars Ehlers PLoS One. 2015; 10(7): e0132421.Published online 2015 Jul 6. doi: 10.1371/journal.pone.0132421
Let’s get one thing out of the way first. The big question overhanging this survey was how representative the 112 people coming from the Danish ME/CFS Association were of ME/CFS patients in general.
The demographic results indicated that with regards to age, gender, and socio-economic status the Danish patients looked much like ME/CFS patients surveyed in other countries. The authors agreed, though, that patients joining a group like the Danish Association probably tended to be less satisfied with their health care, more severely ill and more resourceful than patients not joining organizations like that.
They argued, though, that sampling support groups may actually produce a more realistic assessment than sampling patients from clinics, because clinic studies usually miss the more severely ill patients. Since high percentages of ME/CFS patients (relative to other diseases) are severely ill, the authors proposed that their sampling protocol may more accurately reflect the chronic fatigue syndrome community.
The authors also reported that because they ‘extracted’ the effect of the QOL (HRQoL) of ME/CFS from other conditions that might have been present, the study only estimated the impact of ME/CFS. That was an advance over most QOL studies.
Results
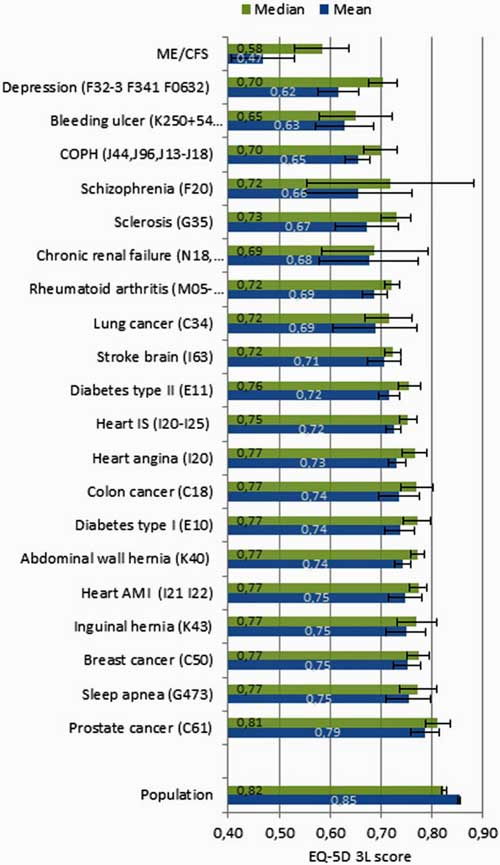
The authors looked at median and mean quality of life scores. The median scores are a more accurate measurement of a community because they’re not skewed by people with really high or low scores.
How did the quality of the lives of people with ME/CFS stack up next to those of people with cancer, multiple sclerosis, heart attack or stroke?
They were worse – significantly worse.
Median Scores
People with ME/CFS had the lowest median quality of life (QOL) scores of any disease tested. The next highest QOL score was 12% higher (bleeding ulcer). Next came people with chronic kidney failure with 15% higher scores.
People with the big, scary diseases ( the ones people think – “Please, Lord not me!”) all had consistently higher quality of life scores than people with ME/CFS.
Schizophrenia is one of the last diseases I would wish on anyone, but people with schizophrenia scored 21% higher in their QOL scores than people with ME/CFS. The same was true for people with stroke, multiple sclerosis and rheumatoid arthritis.
People with Type I Diabetes, cancer or heart problems had it relatively easy. Their QOL scores were 33% higher than those for people with ME/CFS.
Mean Scores
If the median scores were disturbing, the mean scores were frightening. A significant drop in the mean ME/CFS QOL score surely reflected a significant subset of ME/CFS patients, with very, very low quality of life scores.
This time people with the disease with the next lowest QOL score (again bleeding ulcer) were thirty percent better off. People with lung cancer, stroke, diabetes, etc. had almost 50% higher quality of life than people with ME/CFS.
These are incredible figures. Chronic fatigue syndrome is widely regarded as a rather minor disease and its funding reflects that. This study, though, suggests ME/CFS places a greater burden on those afflicted with it than do many of the most serious diseases of of our time including schizophrenia, cancer, stroke, multiple sclerosis and Type I diabetes. Could that really be true?
Time for a reality check.
Reality Check
There was that possible sampling problem. Did the study target a abnormally ill segment of the ME/CFS community? A review of past ME/CFS quality of life and functioning studies suggested the results may have been dead on.
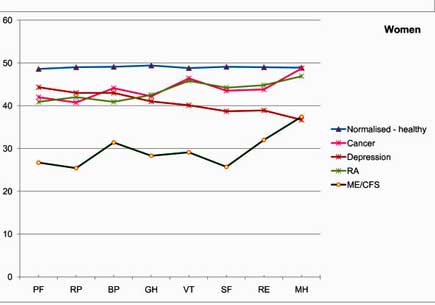
People with ME/CFS had significantly reduced functioning around a broad category of scales compared to other serious diseases. PF = Physical functioning; BP – bodily pain, RP – limitations due to physical problems, GH – general health, SF- social functioning, VT – vitality, RE – limitations due to emotional problems, MT – general mental health.
The results of a 2011 British study comparing functioning in people with ME/CFS vs people with rheumatoid arthritis, cancer and depression showed a staggering reduction in functioning in the ME/CFS patients. Except for emotional and mental health scores – which were similar in depression and ME/CFS – all the functional health scores were dramatically worse in ME/CFS patients.
The most significant study to back the recent findings, however, may still be a large 1996 study by Anthony Komaroff published in the American Journal of Medicine. It compared the functional capacity of 233 ME/CFS patients (from a clinic) with thousands of patients in other disease groups (hypertension – 2,089, congestive heart failure – 216, type II diabetes – 163, heart attack – 107, multiple sclerosis -25 and depression – 502).
Komaroff found people with ME/CFS scored lower than all the other diseases on all the functional scales, again, except for the emotional and mental scales for people with depression.
(Komaroff also found both the degree and kind of functional impairment found in ME/CFS was different from that found in depression. Studies indicate that the scores for the emotional and mental functional subcategories are similar in depression and ME/CFS. What’s different are the far lower physical functionality, vitality and other scores found in ME/CFS.)
Other smaller studies have had similar results. In fact no disease yet assessed has had a greater or even equivalent impact on QOL or functioning as has chronic fatigue syndrome.
A 2011 Italian study found lower quality of life scores in ME/CFS vs hepatitis C. A large 1996 U.S. study found lower physical and social functioning, general health, and body pain scores in ME/CFS patients versus those with acute mononucleosis. In both studies the depth of the fatigue present was the most significant factor in determining QOL.
Children with ME/CFS were found to be more impaired and had lower school attendance than children with juvenile idiopathic arthritis (JIA) or emotional disorders. “Remarkably similar” quality of life scores in three countries indicated that significantly reduced QOL is status quo for people with this disease.
My guess is that QOL issues in ME/CFS are so significant because, besides the sheer discomfort the disease causes, it strikes at the core of who we are as humans. Our nature is to be physically and mentally active. Taking away our ability to work, to socialize, to exercise – is taking away something very precious. Other diseases cause reduced functionality, but few appear to do so on the scale that ME/CFS often does.
These studies suggest that people with ME/CFS get hit harder and in more ways than any disease that’s been tested yet. That was reflected in the incredibly low employment levels found in this study – just 7.6% – and the very high rates of disability (52%).
The NIH’s Stark Choice
This is a rough disease. Functionality and quality of life studies indicate that it’s one the roughest diseases to have. They also provide another set of tools advocates can use to push the NIH and CDC to provide appropriate levels of support.
(If you want a really vivid description of how rough ME/CFS and FM are, check out how ME/CFS and FM patients describe their symptoms in In Their Own Words.): Chronic Fatigue Syndrome and Fibromyalgia Patients Describe Their Symptoms)
The chronic fatigue syndrome community has a lot going against it at the NIH. It has some real ammo as well.
These studies indicate the NIH faces a stark choice. It can choose to support people who have one of the most difficult disorders found, or it can continue on its way and stop pretending that it’s committed to improving the health of all Americans. It can start providing support based on the needs of it’s clients – the American public – or it can acknowledge that it’s an institution that discriminates.
If the NIH can’t finally step up to the plate a different mission statement would be more appropriate:
NIH’s mission is to seek fundamental knowledge about the nature and behavior of living systems and the application of that knowledge to enhance health, lengthen life, and reduce illness and disability….in Americans with the illnesses we have decided to support. (Others need not apply).
Doing Our Part
Every advocacy blog Health Rising puts out over the next couple of months is going to include a request to join the #MEAction project created by Jen Brea and Beth Mazur. The #MEAction project is comitted to being a one-stop advocacy portal for ME/CFS advocacy.
I call your attention to two petitions to increase funding for ME/CFS found on the site. Petitions, by themselves are not going to change anything but they are easy to do and over time, in conjunction with other efforts they can provide evidence of a communities commitment. Please, sign the petitions and join #MEAction.








Your Alternate NIH Mission Statement made me laugh, Cort. If only people/institutions were so clear about their true intentions/priorities. What a lot of confusion that would save!
Martha
Cort, it made me laugh too! And I do think it would be prudent to stop repeating that this disease cannot kill you. There is ample evidence that it can and does. It is just that, like AIDS in the early years, doctors must recognize the true cause of death behind the immediate organ failure or tumor.
Agreed, it’s more accurate to say that it probably won’t kill you. I actually removed that line entirely. Who knows what bottom of the barrel functionality can do to you over time anyway. If it can knock you out that completely….why not more?
Absolutely agree EXCEPT with the statement ME/CFS at it’s worst CAN and frequently does kill.
Why? There are MANY deaths attributed to ME/CFS.
Not as commonly as found in heart disease, cancer, multiple sclerosis, etc. I did misstate, though – – thanks for pointing that out and I removed that sentence from the blog.
I think suicide counts as a “death result,” too, as patients seek a way of ending the suffering, poverty, isolation, and disrespect that piles up as the years move along and we are left behind by life.
Yes, indeed. Of course it does. It says an awful lot.
Brain fog moment – what I meant to say was Absolutely agree EXCEPT with the statement “As has been noted many times, ME/CFS at its worst can do everything but kill you.”
ME/CFS at it’s worst CAN and frequently does kill.
Though many times the deaths are attributed to other causes that the medical establishment takes more seriously and “believes” in.
I guess time will tell on that one. You could certainly be right. Perhaps what counts here is that the feds don’t view it as a disease that causes much mortality and if they did – things might be different. I was told by a lobbyist that if ME/CFS was killing a lot of people he could get money for us in a second.
Why not focus on the causes of this syndrome so that the real issue can be dealt with? I bet a good 90% of the people who are diagnosed with CFS are infected with Tick Borne Infections (TBI). No one even thinks about this possibility. Wonder why not???
Except almost all of us have been tested to death for Lymes and some have even gone through the so called LLMD’s and Inegex? and have not tested positive.
Don’t get me started on the cluster outbreaks of hundreds becoming ill in hospitals and even across miles in the dead of winter.
How do you know it is 90%? I don’t believe this. It would be to ‘ simple’ as a cause for CFS. I do believe some of us could have (chronic) Lyme.
I first saw the local NHS ME clinic when the regional centres were set up. Mine was one of the first. It was a joke. When I became bed-bound I had 3 home visits before they said there was nothing they could do to help me so they wouldn’t be visiting again, & they were removing me from their patient list. I was informed that, once I’d recovered enough to be mobile again, they’d be happy to put me back on the list & see me again. What other illness has “specialists” saying we’ll treat you when you’ve improved but not now, you’re too ill? 😡
I’m not left completely without medical support, I have a wonderful GP clinic, with 3/11 of the doctors taking a special interest in ME & all 3 have requested I be their patient. The first one I saw actually sat in the kitchen with my wife after talking to & examining me. My wife had to make her a coffee & talk to her to calm her down because she was so upset at not being able to do much to help. My wife said the fact she cares enough to want to help & also believes me has been a huge help, which is true. After 20 years abuse from the old GP, being told I was a liar, malingerer, hypochondriac & being repeatedly sent to psychiatrists so often they actually contacted the GP to tell her that, unless I developed new symptoms with a clear psychiatric element, she had to stop wasting their time & mine & not refer me any more. She even broke the rules & discussed my care with my family, telling them I was a lazy liar & they had to ignore me when I needed help. I should have complained but didn’t because I was too ill.
My parents didn’t believe how much of a bitch the former GP was to me, until they saw it themselves. I’d had gynae surgery & given her the hospital letter. I had to go back the following week because the wound was infected. I was refused an appointment when I phoned, being told that we’re not allowed to give you appointments any more, you have to come & wait to see if the doctor will see you. I took my Mum for support. After over 2 hours in the waiting area, the doctor said she’d see me My Mum was hidden behind me as we walked in the door. As soon as she saw me, the GP snapped “What are young going to pretend is wrong with you today? The reception says you’ve had an operation but I don’t believe it, there’s nothing wrong with you. I wouldn’t be surprised if you’d deliberately cut yourself to pretend you’ve had surgery. You’re such a pathetic hypochondriac.” My Mum gasped, she’d always said she was a lovely GP & had never believed me when I’d complained about her, assuming I was simply too sensitive to criticism. I told her I’d given the receptionist the hospital letter the week before, outlining what had been done. She told me it was a forgery so she’d thrown it in the bin. She repeated that I had nothing wrong with me & Mum got angry, saying “I was with her with the gynaecologist gave the diagnosis & discussed treatment. I’ve taken her to every monthly appointment for injections for the last 18 months. Her Dad took her to hospital on the day of the operation at 7am & sat with her until she was admitted onto the ward. We visited her every day until they rang us to say we could collect her to bring her home. She is not telling lies.”
The bitch still refused to examine me so I rang the hospital to ask what to do. They told me to come in & the doctor would see me. I needed antibiotics because the wound was infected. Weeks later I had to go back to hospital because the same GP refused to take out my stitches. I know the consultant wrote to her to make an official complaint about how badly I’d been treated. She replied that I’d never even told her I was ill nor that I’d had surgery. The consultant actually told me this, but he said he didn’t believe her. He said she was one of the dinosaurs who needed to go because they never followed the science, didn’t keep abreast of any advances & basically betrayed their Hippocratic Oath.
My parents eventually apologised for having believed her instead of me. They said because I’d had depression before, they’d accepted what she’d said, assuming it was back. (I had been depressed after being raped. My Dad had been seriously ill at the time, with uncontrollable angina & numerous heart attacks, & I knew that telling them would probably kill him, so I kept quiet, but it destroyed me for years).
After that another GP joined their practice & I only saw her. She was older than the first doctor but kept up with advances. She was the one who said she thought I had ME & referred me to the ME clinic. Of course, when the other one found out she cancelled the referral without telling the nice doctor. After 3 years & numerous referrals I eventually got an appointment but only because the referring GP asked the clinic to refer all correspondence about me to her home address, explaining that there was an issue. Not long after I was told to leave the practice. I should have left long ago but I was so ground down by what had happened, I assumed all practices would be the same. I was wrong.
Bad doctors can destroy people, both from their poor medical knowledge but also their appalling attitude. She destroyed my trust in doctors for a long time, but the GP practice I joined about 12 years ago has certainly restored it. A good GP is worth their weight in gold.
Current research seems to indicate that any long term severe infection can trigger ME/CF/Fibro/PEM. TBD are just one trigger but I agree with you, currently an important one!
i cried as i read your article, Cort. When are they ever going to get it/… my keyboard’s question marks don’t work… i am in Canada, so have followed the news from the States at a bit of a distance. The iom report findings were given to the nih almost a year ago, were they not/ Do we have any idea how they’ve been received, and if the recommendations made are going to be accepted/
i’ve been deathly sick for 14 years, with no treatment at all except for nutraceuticals and compression garments to try and compensate for my failing heart and everything else that doesn’t work anymore. The ignorance of medical and governmental bodies takes my breath … and my hope… away. Thank God for this community.
Christine m.
Reading this reminds me of a Tom Hennessy quote very aptly suggesting the nightmare it is to live with severe ME, with a touch of dark humor: “If you see an ME litterate doctor, he will tell you he has good news and bad news. The good news is this disease probably won’t kill you. The bad news is this disease probably won’t kill you.”
Perfect – that’s what I meant to say but didn’t. Thanks
Tom was good!
that’s what i was told 25 years ago. guilt is the only thing keeping me alive.
This is so true… I know this is terrible to say but I have wished I would get cancer so I could just die. Being miserable every day is no quality of life and if this was a pet we were talking about then they would put down. I thought we humans were above all other animal species but apparently our pets now get better care than we humans. ???
My life is getting shorter and “less” as the days go on. I am now virtually housebound leaving my home for approx 2-3hrs every fortnight. So, i totally get this survey and the lack of understanding & treatment etc in the UK is negligible
Absolutely right Blue Humphries, treatment in the UK is negligible. If you are lucky you will get referred to a “specialist clinic” which could be many miles away meaning painful travel, IF you can get there. Then the best you get is a confirmation of diagnosis, a brief discussion about pacing etc and maybe a handful of follow up phone calls for moral support.
No such thing as an NHS consultant, and the private ones are few and far between and only accessible by those with money. And don’t get me started on the GPs and doctors that STILL don’t even recognise it as a genuine condition, or claim it’s all in the mind. Although to be fair I have found one of the good ones who is very supportive and does what she can, but what is available to her and consequently to me is extremely limited. I have been on long term sick unable to work for over four years so, because of this condition, I barely have enough money to pay the bills. The chances of ever being able to pay for treatment are zero until I am better and can work again. Bit of a catch 22 that.
There are so many truths in this article and STILL it’s all but ignored by many in the medical profession.
Hopefully this study and others are bricks helping build the foundation so that others don’t have to go through this.
For now, though, everybody should know that an appropriations subcommittee just zeroed out half the ME/CFS budget for this year – http://www.cortjohnson.org/blog/2015/08/07/act-now-just-say-no-to-funding-cuts-for-mecfs-research/
Cort (or anyone that knows), sorry, but I don’t fully understand the charts. In the first one, what do the black lines mean? The ones that look like this: |——|
On the second chart, what does PF, RP, BP, GH, VT, etc., stand for?
Maybe I just missed the “key” or maybe these are standard symbols or abbreviations?
Thanks.
PF RP BP GH VT are all different assessments of functionality tested using the Medical Outcomes Short Form Health Survey (SF-36). It’s used to assess the impact of diseases. The abbreviations stand for
PF = Physical functioning; BP – bodily pain, RP – limitations due to physical problems, GH – general health, SF- social functioning, VT – vitality, RE – limitations due to emotional problems, MT – general mental health.
Cort, thanks. That helps. And thanks for all you do!
thank you, thank you! for the question and the answer!
Being a suferer I can believe the findings of these studies. What I personally believe is that support and understanding from the medical community would go a long way in helping the overall QOL of CFS/ME patients. I have been one of the lucky few (UK) who have had long term medical support and it has meant I have maintained part time employment. However I have not been able to get support from occupational health at my work place because quote – “ME is just a label they give you when they can’t find anything wrong with you” and I have had no help from local government in the form of financial aid (I can’t even afford my prescriptions for needed medication) or ablility to get a blue badge to help me stay in work due to blatant discrimination (by the company used to asses for a Blue Badge). Having this illness means you have to fight harder than any other chronic disease just to maintain a life at all which I believe adds to the lower level of QOL for us, fighting for help or recognition in itself is demoralising and frustrating.
Yes you are right Tori. Support and understanding from the medical profession would go a long way to improving our QoL. For instance in my case, I had to fight so hard to get my condition recognised it did not happen until things had got so bad I had a breakdown and had to give up work. I am now having to fight from way down the bottom and the battle is actually harder than ever from a medical point of view.
But it’s not just doctors recognition that is the problem. Because the medical profession still has so much scepticism in it about the condition, that transfers into the working world and society in general. Trying to keep a job is made even harder because employers don’t really understand. Trying to keep any sort of a social life is made even harder because society doesn’t really understand. Trying to manage your finances is made even harder when banks, utility companies etc etc don’t really understand the condition. And perhaps the saddest and most frustrating one is when I recently went the hospital for treatment of yet another ear infection, this time a persistent bacterial and a fungal infection in both ears, and the apparently newly trained doctor asked what other conditions I had then said “CFS/ME, what’s that then”. I can only assume from that comment that they still aren’t being taught about the condition in medical school. Yet in England alone there are known to be over 200,000 sufferers, and that is not counting the ones who are still struggling for a diagnosis.
It’s no the wonder quality of life is such an issue when everything becomes such a battle for people with an already debilitating chronic condition!
Sounds a lot like Lyme Disease. How many of you have been tested for Tick Borne Infections? I have all the same symptoms that come with CFS. I was diagnosed with Lyme Disease. That’s often the cause of CFS, among other things. Is this not something to consider looking into?
Sure it is…I think more people are thinking about that than before.
Yes, I have many times and many others have also. Your doctor did not do his/her due diligence before diagnosing you. Because a Lyme test as well as many other tests are run first.
I have been tested for everything including Cancer, Lyme Disease, etc. So don’t tell me my Fibro and other 14 autoimmune conditions are not real. I was born with at least one of those conditions and my life has been turned upside down since I finally took my husbands advice and switched to a doctor who actually listened and tested me for everything.
Sorry, if my first reply to anything came across as me being upset, but I’m tired of people telling me that my health issues are something else when they are not.
@Nessa – LIKE!
I can’t read the whole study ( Brain fog plus poor english level). But depression being so close with ME in the scale’s table make me wonder if some people ( Drs?) could think that patient’s subjetivity is a key factor in this study ( even if depression and ME are well diferentiated in others studies).
Any thoughts?
This is a very timely subject for me. I have “failed” at so much, over a short time, that I feel absolutely incompetent and embarassed. I have moved to another state to be near my only child who has fibromyalgia and an primary immune deficiency (as I do). She is starting college this Fall. My mother and brother died in 2014.
My rational mind tells me I have done a lot! But, I’ve made costly mistakes that my inner critic screams and ridicules me for over and over. Others are frustrated with me,too.
These studies are good for me to take seriously to set reasonal goals for the “me” that I am, not the “me” I used to be. I think we all mourn for that former self.
I really, really want to get well. And, I how I wish I could lessen my daughter’s pain. She has lived with it since she was 10 years old. She is much kinder to herself and has a greater ability to pace than I do.
I appreciate everyone here for speaking out.
I’d like to clarify: I want both my daughter and myself to get well. And, if only one of us could — I’d give her the opportunity, no question. My comment above comes off sounding different than I meant it.
Good luck Kym. I thin we all struggle with that oh so harsh inner critic. I know I do. I liked what someone said in a Landmark Seminar I was in – if someone came up to you and said to you the things you say to you about yourself – you’d punch them in the face!
One of my goals is just to lighten up a bit – turn off that critic! Good luck with that!
This is a very revealing study showing just how life altering and crushing this illness is. I’m quite sure anyone with ME/CFS would agree with these results showing how serious it is. Now how can this be made required reading for the people in charge of doling out research funding at the N.I.H.? They are in control of a vast budget that the U.S. taxpayers have entrusted with them to use in the best manner. I.M.O. the meager funding of this illness to this point should be considered indefensible by these decision makers and there needs to be an accounting of this. If our illness were to be funded in accordance with the amount of people affected and by how debilitating it is, then the funding should be near the very top – to the tune of hundreds of millions of dollars annually. I fear we are in a forever futile position if we are content in begging for scraps. People making funding choices have been derelict in their duty and need to be taken to task. Studies like this are available for them to read if they are inclined to learn how dire our situations are. What can we do to make sure these people take us seriously?
Many of us have paid taxes for years (and would like to be able to be contributing members of society again) and have expected our $ to be used to fund the most worthy needs. These agencies are designed to serve the people and this is one instance where they have failed miserably for decades.
Thanks again, Cort, for bringing studies such as this to light.
I was diagnosed with CFS 32 years ago. Living in Chronic Pain which hovers around 9-10 on pain scale 24/7. Is Fibromyalgia related to CFS? Most recently diagnosed with Fibromyalgia. (sorry for jumbled words. ..brainfog)
Yes usually if you have CFS, you’ll have Fibro.. many of the same symptoms 🙂 🙁
Erin,
It is my understanding that CFIDS and Fibromyalgia are very similar, related illnesses. I have them both, as well as an autoimmune disorder and arthritis. I have been ill with CFIDS for about 26 years.
The lack of understanding of this illness, even among the medical establishment, is very hard to deal with. Doing one’s own research in terms of daily detoxing, nutrition, activity pacing, etc. has been most helpful for me.
Erin, have you tried capsaicin cream for the pain? It works by blocking substance P, which is elevated in fibro people. I use aloe vera gel along with it, to keep it from burning and itching. Works very well for the pain.
God bless all of you.
Being an MSer myself and my better half being diagnosed with ME/CFS last year, I found this information rather exciting but worrying at the same time.
The exciting part is that ME/CFS is finally on its way to becoming accepted and recognised by society but the worrying part is all the complications an illness this savage can cause.
Do the poor people dealt the ME/CFS card have to collapse before their illness is accepted as REAL!
I don’t think it can be possible that those who have the power to change funding of either research or treatments are ignorant of this kind of research but this is a good study.
I had breast cancer in 2012 and am still waiting for the ‘all-clear’. I can confirm first hand that it was a considerably better experience related to ME/CFS. In my darkest moments – I have prayed to anybody listening – that the BC recurs and kills me quickly. I’m not being dramatic because now that I feel a little better, I am praying that it doesn’t!
I find this interesting but the one thing that bothers me is that Functional scales are patients filling out how they think and feel so how does this prove that the disease is much worse physically especially when you rate it next to cancer of all things. To me this only proves that patients mentally are saying they are feel worse than any of these others on the comparison of functional scales. I have to wonder and I can say this because I am severe but have a very positive and happy disposition in spite of all that is wrong….if this is really more indicative of what this disease does psychologically to the patient then it does physically. And a lot of that may be due to the patients feeling abandoned and ignored and put down. We did functional scales in a group I am in and I had people who could still be up, go out once a week, take care of themselves rated as much lower than me who requires two caretakers. So, I am unsure how to take this report.
And to be honest, I fear functional scales will make them turn more and more to saying this is psychological than physical and that worries me. I have had to fight hard for the care I have but I see that even the SEIDS name change did nothing to change views and worry about this. I do think that this illness dramatically impacts people and especially the severe and mad worse by the need to prove we are sick all the time.
Functional scales are used in all diseases. There’s no reason that I can think of for them to be perceived as psychological in ME/CFS and real in others diseases. There’s no scientific basis to make that assumption that I know of.
My reason for stating that is that it is a subjective test and not one that has anything to substantiate that a person is worse than these other people except for what they say about themselves. I do not think they are psychological. That is not what I said. I said I worried some would look at subjective functional scales and might think the people marking might be embellishing what they mark. I did not say there was any scientific evidence to support this but neither is there any scientific evidence to support what the title says. There are so many variables such as that maybe people with cancer have a brighter outlook on their situation than someone with ME/CFS which would be understandable.
This is not saying that it has been proven that ME/CFS is worse than Cancer, etc. It is saying that the way ME/CFS patients rate themselves they see themselves as worse and I believe that is because of the abandonment of us by the medical community at large and the way doctors and the community at large act about this dx. And that is not referring to the renowned doctors who are working on it. Many of us feel hopeless, many of us feel helpless and that is because of how ME/CFS patients are treated by so many.
That is what I was thinking too. Maybe that subjectivity is why depression is at the second place in the ranking too.
But even so, the subjectivity should be considered real for all the patients in all the diseases I think.
Proving I am sick and tired in my family makes me so much more sicker and more tired from the stress of them not understanding why my husband does so much work around the house . Almost everything actually . It embarrasses me and a few of them have turned against me recently after they found out . They apparently think I am very lazy . I have been hiding it for over twenty years but they recently found out . Can you imagine having to hide something like that ? Not the illness but the fact that I am so disabled . And they don’t look it up they just make assumptions . Also to me looking it upon e does not tell the story anyway . Much research from doctors plus , most importantly the many many many testimonials are what tell the story . I don’t think they would completely believe it anyway cause I don’t often look sick to them .
Hi Cort, first I want to say thanks for all you do here. I also want to ask something I’ve been wondering for a long time. Please don’t take it as a criticism. I am wondering why you use “Chronic Fatigue Syndrome”, sometimes exclusively, as you have done in the title of this article?
Even if you are quoting the title of the original article in your title, I think we can all agree that using the term “Chronic Fatigue Syndrome” really sets the cause of the illness back. Whether you realize it or not you are in a pretty influential position. So, I’m wondering what is behind your choice to use that term, instead of say ‘ME/CFS’, just ‘ME’, ‘myalgic encephalomyelitis’, or ‘SEID’ etc?
I don’t like the term either. I kind of flinch when I use it but I use it in the title and every now and then in the body of the blog for search engine purposes – in order to get the blog as much spread as possible.
Hi, I think perhaps it is time to take a stand against the use of the term “chronic fatigue syndrome”. Please consider that, yes, you are getting more page hits by using it, but unfortunately, and unintentionally, you are aiding in the spread of bad ideas about this illness.
Your blog is very positive for the ME community, don’t get me wrong!! But I think the use of the term CFS provides a net negative impact on the community as a whole.
As a member of the ME community, I’d gladly see less exposure in the short term if it meant I didn’t have to see the name “chronic fatigue syndrome” any more. It does so much damage. It ain’t worth it IMO 🙂
I think not using “chronic fatigue syndrome” might cause short term pain (web hits, media attention/confusion) but will provide long term gain.
I’m praying you will be one of the key players who refuses to use the term and starts a trend.
I think you made a good choice. Hopefully a sceptical doctor might search for chornic fatigue syndrome and come across an article from you such as this one and realize what a serious and devastating illness it is.
I think 99,9% of doctors haven’t even heard of the term SEID yet.
what does SEID stand for?
i believe that the term chronic fatigue still needs to be used. 25 years ago, when i first became very ill, they wanted to change the name. there was an awareness problem back then, as well. so, in my mind, narrowing the field of view would be a mistake.
Systemic exertional intolerance disease I think it is.
You’ve got a point!
As a personal note about the name, or names, I think all of them are stupid. And make things worse, not better, in many cases. However, we’re stuck with whatever someone else plucked out of the air.
About doctors not believing . . . recently I was looking through old (paper) files and came across newspaper article that I had clipped out.
The byline said Daniel Goleman, The New York Times. And the headline said, “Patients who refuse to be well.”
Guess there are still plenty of doctors who think that way? It isn’t just our fault, it’s our fault because we “refuse to be well.”
Breathtaking.
Why don’t we all write a letter to Daniel Goleman? These kinds of statements are devastating for all of us.
I do not think it should be a competition among diseases. Each disease is undesirable. Having that said ME / CFS is a highly disabling disease. It’s the longest and meanest invisible disease there is.
That definitely says something!
Well, funding for ME/CFS just got cut in half so… GAME ON!
A big problem with the name, major problems with funding, severe suffering without understanding from the medical community, mostly the same from one’s family/friends,
can’t really live, 34 years with not a lot of hope on the horizon. Of course it’s depressing, but I fight that thinking, as hard as it is. When I read your comments it gives me hope. I remember the days when there was nothing to read about this illness, and certainly no one to talk to. When I read the words from people who have what I have, it’s miraculous!
Thank you, Cort, and everyone who struggles to express themselves. It really helps. There has been progress—among ourselves.
thank you so much for your efforts in setting up MEAction and all the related online help. just discovered you on 8/8/15 and am sooooooo grateful to have found this forum. {{{big hug}}}
It’s hard for public to judge if they had this disease. Usually we care about the condition of ourself, but mostly we just igorne some signals from our body not so obviously. Is there suggestion for how to tell if someone is with ME/CFS?
I have other autoimmune disease but POTS or CFS or what ever you want to call it is the one that makes my life the hardest by a country mile.
Had this disease CFS over 25years pacing is the best way to get by. Trying gut flora treatment from Natropath. Was bed ridden for two years horrible time funding is a joke any where you live.keep surviving.
Cory could you please send me responses to what I put up ? I would appreciate any suggestions . I meant cort . On my email . Thank you and thanks for this web site . I think I was supposed to check something off to receive emails but I didn’t notice it till I sent in my statement .oh I just checked it ! But not on the previous thing I sent in .
Useful info. Fortunate me I discovered your site accidentally, and I
am stunned why this coincidence did not took place in advance!
I bookmarked it.
I’d love to have a study done showing how many people with ME have the mold gene.