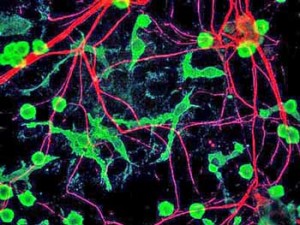
The microglia – key structural and immune regulating elements in the brain – are the green elongated strands
The microglia surround and protect the neurons in our brains and spinal cord. The main immune defenders in the brain, they spew out an array of inflammatory and neurotoxic substances when activated. Theses substances cause the symptoms associated with ‘sickness behavior’ when we have a cold such as fatigue, pain, mental fogginess, etc.
Some researchers believe the microglia have been primed to respond to substances called alarmins that are generated by cellular stress in Chronic Fatigue Syndrome and Fibromyalgia. This microglial hypersensitivity has left them continually activated in Chronic Fatigue Syndrome and Fibromyalgia.
- See Neuroinflammation: Putting the ‘itis’ Back in to Myalgic Encephalomyelitis – Back to the Future for Chronic Fatigue Syndrome?
While several studies suggest microglial activation is happening in ME/CFS/FM, direct evidence that it’s occurring in ME/CFS or FM comes down to just a handful of studies. (The long awaited follow up Watanabe study is expected to be published in the later half of 2020.)
Fibromyalgia Neuroinflammation Finding Could Open New Treatment Options
The list of potential microglial inhibitors below is not intended as a treatment prescription for ME/CFS or FM, but to describe treatment possibilities that future research could indicate are helpful.
The long list of available drugs and drugs under development is, of course, encouraging should this problem be validated in ME/CFS and/or FM.
Possible Microglial Regulating Drugs.
Available Drugs
- Low Dose Naltrexone (LDN) – Has glial cell inhibiting properties and has proven effective in fibromyalgia. Check out Health Rising’s Low Dose Naltrexone Fibromyalgia and Chronic Fatigue Syndrome Resource Center for more.
-
Low dose naltrexone is being studied in fibromyalgia for it’s glial cell inhibitory properties. A different form – dextro -naltrexone – may be more powerful
Dextro-naltrexone – a potentially more powerful form of LDN with fewer side effects. which does not block the opioid receptors. Jarred Younger attempted and failed to get an NIH grant to study dextro-naltrexone in ME/CFS and FM.
- Intranasal insulin – may improve metabolism and is a neuroprotective agent. Many clinical trials are underway assessing the effects of intranasal insulin in neurodegenerative diseases.
- Other intranasals – many other intranasal drugs including some that may reduce neuroinflammation are in the testing stages
- Minocycline – is an antibiotic. In combination with tramadol minocycline was effective in reducing neuropathic pain and IL-1B activity in a rodent model. One minocycline trial for treatment resistant hypertension attempts to reduce sympathetic nervous system activation and enhance parasympathetic nervous system activity – two problems found in ME/CFS and FM. The trial authors reported that “There is no other compound available that is safer and displays specificity better than Minocycline in inhibiting microglial activation. Thus, the potential therapeutic benefits of this inexpensive, well tolerated, already FDA-approved drug that has minimal side effects would be enormous”.
- Dextromethorphan – Mostly used as the active ingredient in cough-suppressant formulations, in animal studies dextromorphan was able to protect neurons from glutamate excitotoxicity, hypoxia and ischemia, and inhibited microglial activation. As with LDN, low doses were more effective and higher doses were not effective in reducing neuroinflammation in one study (using a mouse model).
- Rifampin – a bacteriocidal antibiotic, Rifampin inhibited a variety of inflammatory mediators from microglia including TNF-a, IL-1B, nitric oxide and prostaglandin E2 in a laboratory study. Few other studies have been done.
- Etanercept – Etanercept is able to block the production of a pro-inflammatory cytokine released by activated microglia in the brain. Nancy Klimas is using it to tamp down neuroinflammation in clinical trials for GWI and ME/CFS.
-
Propentofylline – many studies have assessed the effects of propentofylline, a ‘xanthine derivative’. Propentofylline is also being examined for its effectiveness in Alzheimer’s and ischemic stroke. A recent study found propentofylline blocked allodynia in a mouse model.
- Ceftriaxone – another antibiotic, Ceftriaxone has been shown to reduce neuronal hyperexcitability, regulate glutamate transport in the prefrontal cortex, reduce ischemic brain injury and reduce neuropathic pain in rodents.
- Glatiramer acetate – Glatiramer acetate or Copaxone is an immunomodulatory drug which has been shown to reduce microglial cell activation in M.S., modulates TNF-1 and IL-10 expression in microglial cells and is believed to have other neuroprotective properties. One person with ME/CFS did great on Copaxone until she became allergic to ti.
- Ibidulast – the fact that ALL the Ibidulast studies (except one) in the Clinicaltrials.gov database are recruiting indicates how new the drug is to the medical establishment in the West. Of the 9 studies underway two focus on multiple sclerosis and one on microglial inhibition in migraine.
Check out the latest on Copaxone in ME/CFS
Copaxone – Could a Multiple Sclerosis Drug Help with ME/CFS?
Supplements
- Cromolyn – a Boston company has reformulated cromolyn, a mast cell stabilizer, so that it can reach the brain. It has begun a large clinical trial.
- NAC – recent studies suggest that n acetyl l-cysteine, a precursor of glutathione, the major antioxidant in the brain, is able to make it past the blood-brain barrier. Shungu used it in a small ME/CFS clinical trial (results unknown).
- Resveratrol
- Intranasal glutathione – has shown some promise in Alzheimer’s in increasing GSH levels in the brain.
Are Intranasal Drugs the Future for ME/CFS and Fibromyalgia?
Drugs Under Development
- The Michael J. Fox Foundation has created small molecules which in early trials reportedly stopped neuroinflammation in its tracks in Parkinson’s disease. It hopes to use them to create drugs.
- The Cure Parkinson’s Trust in the U.K. is repurposing three cancer drugs that it believes may help halt the neuroinflammation present in Parkinson’s,
- PTI-125 – – is a drug with reportedly “powerful anti-neuroinflammatory effects”. PTI 125 appears to reduce the levels of neuroinflammatory markers in the cerebrospinal fluid. Cassava Science’s phase IIb trial of PTI 125 began in 2019 with NIH funding.
- XPRO1595 – INmune Bio is developing XPro1595, a biologic drug it hopes will stop chronic inflammation by neutralizing the soluble form of the proinflammatory form of TNF (sTNF).
- BPN14770 – targets an enzyme that increases neuroinflammation. A Phase II trial was underway in 2019
- 3-hydroxymorphinan
- Dilmapimod – in clinical trials for neuropathic pain
- ATL-313
- Bay 60 – 6583
- FP-1
- Resolvin-D1 and EI
Botanicals
Jarred Younger has been studying a wide range of botanicals. The Michael J Fox Foundation is testing “a novel series of plant-derived compounds with high “anti-inflammatory activity” that have been structurally modified to reduce neurotoxic inflammatory factors in the brain.
-
Cucurmim
- Luteolin
- Resveratol
- Gastodia Elata
- Obovotal
- Inflexin
- Pipera kadsura
- Ganoderma lucidum
- Berberine
- Isodon japonicas
- Epimedium brevicornum
- Stephania tetranda
- Stinging nettle
- Fisetin
- Pycnogenol
- Boswellia
- Kratom