



In this second of two studies by Stanford researchers on low dose naltrexone’s effectiveness in Fibromyalgia (FM), LDN was found to significantly reduce pain and improve mood and quality of life. About 60% of study participants reported pain reductions of at least 30%. Sleep and fatigue were not affected. The second study, a small placebo-controlled, blinded cross-over study, was a followup to a smaller less rigorous but successful first study three years ago.
Pointing to the three drugs already approved for FM, the researchers suggested LDN as a possible fourth.
No LDN studies have been done in chronic fatigue syndrome (ME/CFS) and none are underway, but it’s the first drug Dr. Klimas, a prominent ME/CFS physician, turns to for pain in ME/CFS and fibromyalgia.
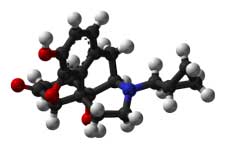
Low Dose Naltrexone
Usually used in high doses to combat alcoholism and narcotics withdrawal, low dose naltrexone is being examined in a variety of disorders including fibromyalgia, multiple sclerosis and schizophrenia. LDN blocks the opioid/endorphin receptors in the brain and has the advantage of being cheap (@ $40/month), readily available and safe.
LDN been used in fibromyalgia and chronic fatigue syndrome and other disorders for years but only lately have studies begun to examine its effectiveness. Cheap, unpatentable and readily available at compounding pharmacies, LDN is no gold mine for drug companies but could be a boon for patients on a budget.
Despite the lack of interest from drug companies, 23 LDN drug trials are underway on disorders ranging from fibromyalgia to multiple sclerosis to alcoholism to Crohn’s disease to Schizophrenia. The American Fibromyalgia Association funded the two Stanford low dose naltrexone fibromyalgia trials.
Why Low Dose Naltrexone Might be Effective in Fibromyalgia or Chronic Fatigue Syndrome
LDN could be reducing pain and improving mood in several ways.
Endorphin Release – By blocking the receptors for endorphins, one of the ‘feel good’ substances in the brain, low doses of naltrexone appear to trick the brain in producing more endorphins. Given that endorphins are known as ‘natural pain relievers’ some of LDN’s effects in FM could be from endorphin related pain relief. Several studies suggest altered endorphin levels are present in the brains of people with fibromyalgia.
Endorphins are produced by the HPA axis, which is impaired in both ME/CFS and FM, and during such activities as exercise, meditation, sex etc. all of which are probably fairly rare in people with these disorders.
Natural Killer Cell Stimulation – LDN enhances the responses of natural killer cells, an area of much interest in ME/CFS.
B-cell Inhibition – LDN inhibition of B-cell activity is intriguing in light of the Rituximab findings and the LDN studies underway in autoimmune disorders such as multiple sclerosis.
Mouse studies found LDN provided a ‘remarkable neuroprotective effect’ on mice engineered to have autoimmune encephalitis. One third of the mice, for instance, injected with LDN did not show any signs of neurological disturbance (compared to 100% of non-injected mice), and disease severity was greatly reduced overall.

Glial cells in the central nervous system. Microglial cell activation could be contributing to the pain and fatigue in fibromyalgia and to the neuroinflammation found in other neurological disorders.
Microglial Cell Inhibition – The Stanford researchers believe fibromyalgia is a neuro-inflammatory disorder characterized by ‘hyper-sensitive’ microglial cells; the main immune cells in the central nervous system.
Structurally similar to the macrophages found in the body, resting microglial cells display little activity but transform themselves, after being activated by inflammation, infection or cell death, into ‘hairy monsters’ that spew out pro-inflammatory cytokines, excitatory amino acids such as glutamate and nitric oxide with glutamate being a primary agent of damage. (Interestingly, glutamate production appears to be associated with reduced glutathione levels that occur during microglial activation. )
Microglial cells are responsible for producing neuropathic pain and flu-like symptoms such as pain, fatigue, etc. (eg sickness behavior). Rodent studies suggest LDN blocks the activity of toll-like receptors (TLR4) found on the microglial cells .
New Drug Target
Microglia produced neuroinflammation could be contributing to a wide variety of neurological conditions including multiple sclerosis, Alzheimer’s, traumatic brain injury, Parkinson’s disease and others and researchers are beginning to explore ways to keep microglial cells from becoming over-activated. The authors of this study stated they expected that new compounds aimed at keeping microglial cells quiet are under development and being tested.
Unfortunately it’s impossible to directly assess microglial functioning in humans but recent advances in positron emission tomography may be peeling away some of the fog currently veiling microglial activity in humans.
A New Class of Neuroprotective Drugs?
LDN is not the only possible microglial inhibitor that might work in FM or ME/CFS. Other possibilities include naltrexone’s close relative naloxone, dextromethorphan, 3-hydroxymorphinan and ibudilast. Each of these drugs was developed for other purposes and later found to have microglial inhibiting properties and the optimal doses for each, interestingly enough, is likely to be much lower than suggested for their original purposes.
In fact the authors propose that finding the correct dose will play a key role in how effective these drugs are. The authors expected that testing was probably underway to determine that.
Conclusions
LDN’s availability has kept drug companies from pursuing it but it’s an intriguing option in Fibromyalgia and ME/CFS. It’s no panacea and the latest study suggested it may not be effective against fatigue but chronic fatigue syndrome is also a pain disorder and LDN’s ability to improve mood and quality of life would be welcome indeed.
Compounding pharmacies are pharmacies in which some drugs are mixed and produced on site. Drugs can be tailored to an individuals needs using the compounding process.







I have been taking LDN for 19 months for my fibromyalgia chronic fatigue syndrome I do say it does help the pain but it did not help the fatigue as much as I wish it would’ve and I will be on LDN for life as far as I’m concerned… I wish everybody had a chance to try it. Not many doctors know about it or care to learn so if you want to try it on your own there is a way go to LDNscience.org Read up on it there is a link on how you can get it to find a doctor that uses LDN
Thanks for the link Renee – I’ll put it on the main LDN page. Glad to hear that it’s been helpful….
was wonderin how u r doing on it a yr since ur log in (feb 2013) and what mg u take? i am waitng on mine to arrive in the mail from canadian rx!! I ve tried everything this HAS TO BE IT!!
Cort,
thanks for the informative post. what is your reference for your statements…….
Natural Killer Cell Stimulation – LDN enhances the responses of natural killer cells, an area of much interest in ME/CFS.
B-cell Inhibition – LDN inhibition of B-cell activity is intriguing in light of the Rituximab findings and the LDN studies underway in autoimmune disorders such as multiple sclerosis.
…….i’d like to peruse & use those references.
thanks,
I take very low dose naltrexone (between 0.5 and 1.5 mg) in the morning (less vivid dreams). This is my third try. The first 2 times I started at 0.5 mg and slowly increased to 4.5 mg over a period of 5-6 weeks, then I got an infection (cold, ….) and it didn’t work anymore. Now I take it 5 days a week and between 0.5 and 1.5 mgs for the past 6 months. I didn’t have a real cold or infection since then (a couple of days with dry throat, a few days of sniffing, 2 days of coughing, but that’s it) I have less dizzy spells. Instead of getting dizzy after a 12-15 min walk, I can now walk 25-30 min. A bit less digestive problems and a bit more regular bowel movements. A decade of CFS has made me very careful, LDN makes me a bit more daring. Overdoing it results in less severe PEM; 2 days of taking it easier instead of 3-4 days homebound. Can’t say I noticed a real improvement cognitively. Not good enough to get me back to work, but definitely quality of life improvement.
Hi,
I live in Fla and cannot seem to find a fibro specialist to prescribe ldn for me as it is not FDA approved. How can I purchase this as I am in terrible pain and this medicine sounds so encouraging.
plz use ldn 4 fibro in the Subject box or ur mssg will go to spam.
many tnx,
RJ
You might want to check out the LDN website and see if they have some suggestions. If you’re near Miami, Dr. Nancy Klimas and Dr. Reye use LDN frequently
Root Causes Ft, Meyers.
Great team.
I have ME. I tried LDN recently during four weeks. I have never been so active for many years. It was like I managed to do as much in two weeks as I would do in one whole year. I had to limit the dose to 2 mg because otherwise I had to much headache. A common problem for me is that I get intolerant to drugs and naturopathic drugs, after a few weeks. This also happeded to me in this case, so I had to finish taking LDN after around four weeks.
I have never had such a great increase in activity ability for any treatment except for a time when i tried NADH. Unfortunaltely, I became intolerant that time also, I finished taking it and felt very bad afterwords. I even think I got some permanent damage from the test.
I take metylcobalamin and kutapressin also. Methylcobalamin does not really increase the ability of physic activity, but reduces symptoms and mental fog. Kutapressin does neither increase physical ability, but reduces malaise, feeling awful, pain in the head, so it eases the burden of having ME.
My experiences:
Increasing the dose too abruptly causes problems. For me I think increasing in steps of 1 mg each week would be adequate. Rapid increase I think cause nightly sweats, stomach pain, and headache. Basically the same as the side effects described on the packing list of naltrexone.
I had a small glass jar of about 100 ml (1 dl) with lid, where I added distilled sterlized water and half a tablet of naltrexone. I put it in the refrigerator. When the ½ tablet had dissolved, I shook the jar so the tablet residues detached from the bottom. A half tablet contains 25 mg of naltrexone and if one uses 25 ml of water, the concentration is 1 mg/ml. To have 4 mg of naltrexone, one sucks up 4 ml of liquid. One can use a regular 2 ml syringe.
Maija Haavisto description of LDN for ME:
http://www.fiikus.net/?ldn
Video (4 min) showing how LDN acts on a cellular level:
http://youtu.be/z0p0ykSzy9o
Thanks Erik, too bad you couldn’t stay on the drug. I have had similar experiences. Thanks for the great references, though; I will put them on the LDN page.
Great article again Cort. If only we knew the particular damage in the CNS to home in on.
I had written a comment but somehow dissapeared.. (maybe I forgot to submit 😉
Forgot what it was, but at least about that I know that LDN is worthwile to try and what I referred to is that I’ve known LDN for it’s great results with MS. Interesting info – also about the background of LDN – in this link: http://www.lowdosenaltrexone.org/ldn_and_ms.htm
Too bad you Erik and Cort couldn’t stay on LDN due to the bad drugintolerance. It’s always frustrating when you can’t keep on your meds simply because your body can’t handle them, know it all to well. I don’t know if it will do anything about that specifically, but I do know it can help considerably with intolerances in ME in general and I think drugintolerances are included. It’s the Far Infra Red, also recommended by dr. Myhill. It eliminates toxins, improves oxigenintake, improves organfunction etc. It’s a special regime that needs to be tailored not to overload your body and get an adverse effect and therefor not recommended to do without guidance!
It’s the light – not the heat – that does the trick, it’s developed by NASA and one of the firm that dr. Myhill recommends and I have experience with (also because I wanted to be able to use certain meds because of drugintolerances that made me had to stop often before) has very experienced people that have used it themselves for years and know a lot about it. They have great experiences with it from their customers and can also help you with other things that are suitable in a persons specific situation or general things (like probiotics developed for the cold war that can do a lot for the gutdysbioses we all suffer from).
It’s not cheap, so not for everybody unfortunately, but well worth to check out if you can afford it. http://www.drmyhill.co.uk/wiki/Detoxing_-_Far_Infrared_Sauna_%28FIRS%29 Get Fitt is where you can get the gentlest and most efficient way of using it, with very good service and guidance and being able to get the best results. It’s no quick fix, but worthwile in many ways and might help you be able to go on and stay on LDN. Wanted to let you know.
Thanks Monique, I never tried LDN actually but I have had a problem with drug and supplement tolerance. I love saunas, had a great experience with one temporarily but it was too much for me to do regularly so I’m interested in the Far Infrad red ones for sure. In theory saunas are the kinds of things I would do regularly if I could. Thanks for the tip and thanks for the link.
Yes, drug- and supplementintolerance is a big problem for us. Ironic too, that what might help us get a bit better, makes us even worse.. Sauna’s are way too intense for us, even infrared ones, unfortunately. The great thing about Far Infra Red is that it’s not the heat that does the trick, but the light and most people don’t even get to the sweating (which isn’t necessary for it to have effect) for months or longer, because you have to start low and over time, depending on your response, very gently increase time and temperature.
I am on it for 1 month now, the temperature I’m on is just a 30 degrees celsius (86 fahrenheit) (was 32, but even gave me too much and too long increase on symptoms) for just 30 seconds a time (was 1 minute, but was too much as well). And not even the 3 times a week, but much less. It’s different for everyone, that’s why individual monitoring/guidance (this is done by phone/skype) is so crucial with this. But even those low temperatures and very short sessions in their experience can have great effect!
Ah – neuroprotective – great but why needed – from what ???
It seems to fall to us (well you) to bring the mass of research findings into a single understanding.
From Tom – a warning..Tom appears to have taken a higher dose in the beginning that suggested and it had really negative effects.
But, PLEASE be VERY careful if the patient has been on Opiate pain meds! I have been on Opiates DAILY for 25 years. EVERY damn Day. except for ONE month, when i went through a TERRIBLE, BRUTAL detox, that SNAPPED off a TOOTH in the hospital, and 5 WEEKS later, i was told to take ONE 5 Mg. Naltrexone pill and i put that in an 8 Oz. glass of water, THEN i was told to take A single Dropper of fluid and take 20 Drops of the 8 Ozs of water with ONE crushed up 5 mg. LDN tablet, and then put THAT 20 drops of liquid into an 8 oz. glass of water, and BOOM….i started heaving and throwing up for 12 hours straight!
I know that Dr. Nancy Klimas is Dead sent against giving Opiates to her pain patients…..but i was throwing up Continuously for 12 god damn HOURS…and finally, at 2 am, i decided to DRIVE to Miami and be at Dr. Klimas’s office in the Morning and DEMAND to go back on Opiates…and after 45 minutes of driving south, i got too exhausted to drive anymore and i turned around and headed back up north, and i must have fallen asleep around Sample road, 20 minutes north of Fort Lauderdale, and BOOM….i fell asleep with NO discernible drugs in my system and i hit the back of a broken down Semi-trailer,,,,FULL blown 18 wheeler and came within 1/3 of an inch of taking my head off! and 5 more damn years of Nursing homes and MORE fentanyl Patches and now, i am back FIGHTING for my life….EACH and EVERY day…..so be VERY careful on recommending LDN IF the patient is taking Opiate meds for PAIN!
Just a word to the wise!!!
I cannot take opiods. Or any other pain med. I cannot/do not metabolize anyyyything as do ‘normal’ people. No SSRIs, no anticholinergics, no anesthesias, no caffeine, not even sugar. I cannot drink a sip of alcohol without passing out. There is virtually no med without the potential to kill me. Hence, the prevailing consensus is I am not sick but nuts. That is right up until a doc sees me cold as ice on a morphine drip and says in a low and urgent voice, “We are losing her, dc the IV and get her out of here”….He had no idea that I could hear him. When I broach the subject of med metabolism with ANY physician, I get interrupted and told, ‘Welll, everyone ELSE takes it” . They blame the patient as if we were suffering and trying to die to ruin their day. They can blame the victim allll dam day long but that does not change the fact that they are not only failing to help us, but dangerous to us. Something is very wrong with us, and I am beginning to think that science really doesn’t want to find out what it is. I keep thinking about the money in drugs and arms…the big money that runs the world. I don’t think about kind, dedicated interested physicans. I think drug dealers. And I need…a NEW drug.
Oh, yeah, there is a name for this, lol. “Slow acetylator” . But is the following the WHY of OUR ( my condition) as exagerrated as it is ? Google it and learn more. If you know sometthihing about this, I am eager to learn. And btw..I cannot do saunas either. Or sun. Or cold. Or…lol…anything.
http://wiki.answers.com/Q/What_is_slow_acetylator
A slow acetylator is a person who has an recessive single gene trait which effects the N acetylate transferase enzyme in the liver. This gene causes the enzyme to work slowly in the metabolism of certain drugs. Because of this slow pace situation the slow acetylator person will receive more of the given drug in his general circulation than a fast acetylator who is metabolizing the drug and sending it out of his body via the kidneys and urine at a quicker rate and thus leaving a smaller amount in the general circulation,i.e., bloodstream. The fast acetylator is in the optimum situation. (It is better to be fast than slow in drug metabolism.)
What to do?
There is now a simple test that can by pass genetic testing for the acetylator gene. It involve some sips of coffee and a tracing of the coffee’s metabolic residue in the urine and the amounts and rate thereof. Or one can just have the DNA tested. Or in the more time honored fashion the doctor can simply adjust the drug dosages until the tolerable level of side effect if any is reached.
Slow acetylation does not mean drug allergy per se and does not rule out the taking of prescribed drugs.
It effects up to 50% of the population in certain groups, Canada and Germany for example and as low as 10% among some American Indians.tylator
I was given that terminology ‘slow acetylator’ by a doc…no testing required in his opinion. But I’ve a hunch that given slow acetylation AND whatever CFIDS is, there is something much more malevolent/dangerous going on in our systems.
Yeah, try mercury – it poisons your mitochondria and slows down everything – including enzyme production. Do some research on it – you’ll be suprised at the exacerbating effects it has been proven scientifically to have on CNS/brain injured people that present with the many neuroimmune diseases we have seen cropping up in modern times.
I in hospital just now coming off opiates tried everything from morphine to methadone. I am atarting on ldn then I pinning my hopes on it. X
Good luck lorna!
I have fairly rapidly weaned off Mscontin. My Dr is dragging his feet per pharmacist with microgram doses. I am in so much pain I don’t think I can tolerate this much longer. I need to get to therapeutic dose to even see if this works for me. Someone TELL. ME ITS WORTH IT!!!!
Hi Pat
It is worth it. I was a wreck with the pain and the slow start with the LDN… It was well worth it! I am now able to do in an hour what took a day. My life is no longer based upon severe pain and tolerating. It is now like a normal persons for the most part.
Today I worked a full day, worked out for 45 minutes, went shopping and am here studying for a course. In a little bit I’ll start cooking a full meal.
A month ago I would have been sobbing and praying for the pain to abate. Now I pray in thanksgiving for a new lease on life. Hang in there! Honest !
Great to hear V – Congratulations 🙂 and thanks for passing it on…
where was ur fibro pain the worse? that LDN took pain away?
Clarification. Microgram doses of naltrexone
What are some other tlr4 antagonists? I came across these below.. Also amitryptyline, ldn (naloxone and naltrexone).
I suffer from some airborne particle landing on my nasopharynx which the goes from afferent vagus, to the solitary tract, to autonomic dysregulation. Only NSAID (ibuprofen specifically) and klonopin help. I also read some articles connecting binge drinking and tlr4 receptor hypersensitivities.
Anyone have any other thoughts on reducing tlr4 expression in the nasopharynx? Or in the upper airway or distal esophagus? Thanks – Tom
Table 2: Mode of action of various molecules targeting TLR4.
Molecules interfering with TLR4 and TLR4-mRNA expression
(1) Chloroquine
(2) Ketamine
(3) GTS21 (nicotinic analogue)
(4) Statins
(5) Vitamin D3 (?)
(6) Lidocaine
(7) Glycine
Molecules interfering with TLR4-related intracellular signalling pathway
(1) Eritoran (E5564)
(2) Resatorvid (TAK242)
(3) Ketamine
(4) Opioids
(5) Vitamin D3 (through its action on LL37)
(6) Lansoprazole (through its action on SOCS1)
Very interesting, Tom. What an interesting group of drugs! Thanks.
So, what’s the normal LDN to start at and to finish at? I just had a pharmacist give me a cost of $125 for 100 of the .5mg pills. I’m thinking that making it up myself by dissolving the tablet would be much more cost effective. Also are there many side effects?
There are little to no side effects. You may have some sleep disturbances for the first few nights. I take mine right before I go to bed, so I am asleep before it kicks in. You may have some vivid dreams. I take LDN for MS and it has been amazing for me. I would recommend giving it a try. There is a compounding pharmacy in Boca Raton Fl that will fill a 3 month script for less than $60/shipped. I wish I could be more help on what dosage to start at, but I don’t know what works best for your condition. I started at 1.5 and I am on 2.0 now. I am getting ready to increase to 2.5. My optimum level should be around 3.0-4.5. I think this is consistent with most conditions. I wish you many pain free days and hope this info helps.
Thanks for sharing your experience Crystal. Glad it’s been helpful for you.
I’ve been taking 4.5mg of LDN for the past 2 years for Hashimoto’s and the associated joint pain. My antibodies have gone down significantly and the joint pain has gone. It’s been a wonder drug for me.
Hello
The article refers to LDN as being a low cost option for those on a budget. Namely $40 per month. What dosage per day would this be for please?
Kindly, Jane in Australia (Nov 2018)
PLEASE CORT,Can you help me.Im in Australia and have severe ME/FIBRO. severe pain
I was on a cocktail of opiates . Fentynal patches,tramadol and panadeine forte. I weaned of the tramadol. Then I went to a specialist who told me about LDN. I cut down the patches and forte for a month then stopped altogether. I then went through a living hell on earth in my own bedroom. The pain spasms and stomach cramps were indescribable. I could eat or sleep. It is now day nine and I can only eat very small amounts,BUT my pain is still so intense and I can hardly stand/dizzy and intense pain. I started the LDN 3 days ago 1.5mg twice day. Is this too much. Im very desperate for any advise Please!
My doctor told me about this Low dose Neltrextion today . But he explain to me a little bit about it and also told me to read about it some more. I’ve read this comment that some says it will works to treat Fibromyalgia . I’ve been having Fibromyalgia for about 8 years. I hope this medication will work for it. Also if someone was taking this to treat for Fibromyalgia and it works pleas tell me some more. I’ll be glade to know about it.
Thanks
i have cfs and very painful fibromyalgia, i want to try ldn and gotten two opinions on it. i take tramadal over a 24 hour period no more than 3003 to 35o mil. dr. teitellbaum wrote me and said that i can still take ldn and the tramadal yet the literature says no. have anyone ever used ldn and tramadal and not had side effects?
Jacob Teitelbaum, M.D. wrote:. If on 300 mg of tramadol, I would still consider the LDN. Sometimes I use the Lyrica just at bedtime as it helps sleep, and at 250 mg the sedation is usually gone by
does anyone have any thoughts on this?
help in denver
leslie