



“The long term follow-up of FMS patients indicates…..that the degree of improvement achieved by many medications…is modest at best” Ablin and Buskia
Affecting 2-3% of the population of the US or about 8,000,000 people in the US fibromyalgia’s impact is huge yet physician ignorance is high, with many doctors restricting their drug prescriptions to the three drugs the FDA has approved for fibromyalgia.
The Mayo Clinic – which appears to set the standard for brief, pithy and unrevealing treatment prescriptions for FM and chronic fatigue syndrome – lists just three categories of FM drugs; NSAID’s, anti-depressants and anti-seizure drugs. Adding muscle relaxants, pain relievers (tramadol, opioids) and benzodiazpines to the mix, WebMD does better, but that list, as a recent review article focused on possible FM drugs indicated, is still far too short.
If Ablin and Buskila are right, many doctors are just scratching the surface of the drug possibilities for fibromyalgia. With all the misery present in FM, it’s not acceptable that doctors are not aware of the all drug possibilities present.
(In fact, with their emphasis on the central nervous system affecting drugs, Ablin and Buskila are certainly underestimating the drug possibilities for FM as research uncovers problems in the periphery (e.g., muscles, skin, immune system) as well. The finding that small fiber neuropathy may be common in fibromyalgia, for example, shifts the treatment focus in an entirely different direction, to the immune system and intravenous gamma globulin (IVIG).)
The review article is called ‘novel therapeutic agents’ but many of the drugs in it received one or two studies in the past. These ‘novel agents’ are mostly promising drugs that need more study.
The ‘Novel’ Fibromyalgia Drugs
Norepinephrine Reuptake Inhibitors (NRI’s)
- Esreboxetine – the dogma in FM ‘antidepressant’ use is that serotonin and norepinephrine reuptake inhibitors work better than serotonin or norepinephrine reuptake inhibitors, but two studies suggest that the NRI esreboxetine can be quite helpful. A large (n>1,000 people) randomized, placebo-controlled, blinded study found esreboxetine produced significant reductions in pain, fatigue and fibromyalgia impact scores. (Note that studies indicate antidepressants can reduce pain in people without depression.)
Dopamine Receptor Agonists
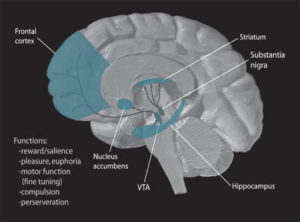
A neurotransmitter most known for its ‘reward enhancing’ factors (and the role it plays in drugs like cocaine and amphetamines), dopamine also opens up the blood vessels (a vasodilator), is an immune modulator (reduces activity of lymphocytes, reduces food flow through the gut (gut motility), reduces insulin secretion and more.
Attention deficit disorder, restless leg syndrome, Parkinson’s disease and schizophrenia have all been associated with dopamine dysfunction. Low dopamine levels are associated with many symptoms common to fibromyalgia and chronic fatigue syndrome including stiff, achy muscles, tremors, cognitive impairment, difficult focusing, poor balance and coordination, a walking pattern characterized by talking small steps and impaired fine motor skills.
- Pramipexole – greater than 42% of FM patients achieved a greater than 50% reduction of pain in a 2005 study. Visual analogue pain scores were reduced by an average of 36%. Lesser improvements in function and fatigue were found.
Substance P Antagonists
A neurotransmitter that increases pain, substance P levels are increased in fibromyalgia, making it (and its receptor) an intriguing drug target. (Receptors found on the outside of cells or soluble receptors in the bloodstream react with a substance (such as substance P) to initiate change (such as increase pain). Reducing substance P receptor levels would, therefore, reduce substance P’s effects on the body.
Substance P antagonists have been investigated for their use in reducing nausea during chemotherapy, as antidepressants and in reducing pain. A safety review indicated they were generally safe and well tolerated.
- Casiopitant (Rezonic) – knocks down the receptor for substance P (neurokinin-1). A Casiopitant FM trial ended in 2008 but the results have not been published.
- Aprepitant – the review does not mention aprepitant, the only substance P antagonist used in clinical practice. New substance P inhibitors are under development.
Opioid Antagonists
“More extensive use of opioid antagonists as well as the introduction of novel microglial activation inhibitors (miRNA) pose exciting new possibilities for the treatment of FMS” Ablin and Buskila

Opioid antagonists may be able to relieve pain for some with FM by turning the activity of the opioid system down
It may seem strange to target drugs that knock down one of the main pain inhibiting systems in the body but the opioid receptors in many FM patients appear to filled and elevated opioid activity in the brain can cause increased, not decreased pain sensitivity.
- Low Dose Naltrexone (LDN) – An opioid antagonist long used by people with fibromyalgia for relief, LDN finally got a clinical trial and it was successful. At the low doses used in the trial, Ablin and Busklin suggested LDN’s effectiveness in FM may have been more due to anti-inflammatory effects than to opioid antagonism.
- Dig Deeper! Low Dose Naltrexone and Fibromyalgia
- Dig Deeper: Successful Low Dose Naltrexone Fibromyalgia Trial Points to Safe, Low Cost Therapy; Implications for Chronic Fatigue Syndrome Dose Naltrexone
Cannabinoid Drugs
One theory suggests the endocannabinoid system in the body is simply not up to snuff in fibromyalgia, chronic fatigue syndrome, IBS, migraine and other disorders. This major system, which is found throughout the peripheral and central nervous systems, plays a key role in pain reduction and has strong anti-inflammatory properties.
A review of cannabinoid use in non-cancer pain found that fifteen of eighteen trials “demonstrated a significant analgesic effect of cannabinoid as compared with placebo and several reported significant improvements in sleep. There were no serious adverse effects. ” Cannabinoids were described as usually ‘modestly effective’ in treating neuropathic pain.
(On a personal note I’ve found medical marijuana to be effective in reducing pain, enhancing sleep and as a stress reducer.) Dr. Clauw has said he would readily swap out cannabinoid drugs/medical marijuana for opioids and other drugs if they were available. Different kinds of medical marijuana can have different effects. We’ll have much more on cannabinoids and medical marijuana later.
- Nabilone – is a synthetic cannabinoid often used to treat nausea during chemotherapy. Nabilone improved pain and functional capacity and reduced anxiety in FM in two studies and improved sleep (but did not effect pain in one).
- Dig Deeper! Check our new Nabilone and Fibromyalgia Chronic Fatigue Syndrome (ME/CFS) page
NMDA Antagonists
Located in the dorsal horn of the spinal cord, the NMDA receptors are found in prime territory to regulate pain symptoms. Dorsal horn neurons receive and filter sensory information from all over the body and then transmit it to the brain. Over activation of these neurons has been shown to participate in producing hypersensitivity pain states (central sensitization). This suggests that toning down the NMDA receptors on these neurons could turn down pain levels, as well.
- Dextromethorphan – A 2005 study indicated dextromorphan reduced a key part of the process (windup) believed to produce central sensitization in fibromyalgia. Thirty percent of FM patients responded ‘positively’ to dextromethorphan in another.
- Ketamine – Several studies indicate Ketamine can reduce pain in fibromyalgia. See our Ketamine and Fibromyalgia page.
- Memantine (Axura, Akatinol) – Studies indicating raised levels of glutamate in the insula, hippocampus and posterior cingulate cortex regions of the brains of FM patients have ignited interest in Memantine. Memantine is a new class of drug that blocks glutamate from exciting the NMDA receptors believed to contribute to central sensization…Memantine also enhances dopamine activity. A fibromyalgia memantine trial should be getting underway soon.
- Dig Deeper! Check out our new page on Memantine, Fibromyalgia and Chronic Fatigue Syndrome
R-HT3 (Serotonin) Receptor Antagonists
Depending on where it’s produced serotonin either enhances pain or diminishes it. 5-HT3 receptor antagonists attempt to diminish serotonin’s pain facilitating properties. 5-HT3 receptor blockade may also be able to reduce several immune factors that may be important in ME/CFS/FM including TNF-a, IL-1b, IL-6 and fatty acid derivatives called prostaglandins that may be increased in ME/CFS.
- Dolasetron – forty-two and 28% of FM patients in one trial had greater than 30% and 50% decrease in pain. Reductions in fibromyalgia impact, anxiety and depression were not significantly different.
-
Tropisetron – Tropisetron not only helped to normalize cardiac autonomic nervous system functioning but reduced ‘pain perception’ as well in a 2007 study. Forty-five percent of patients in a large 2004 trial reported having ‘good’ to ‘very good’ results in a large 2004 retrospective study. Fifty percent of FM patients in a small trial reported Tropisetron had a good or very good influence on their pain. Serum substance P levels droped in the responders. Reduced activation of brain regions associated with pain production was found in another small Tropisetron study. Forty patients of FM patients reported a greater than 35% reduction of pain in a large 2001 Tropisetron trial. The number of tender points and sleep and dizziness were significantly improved. Tropisetron also has neuroprotective, autonomic nervous system, immune modulating and sensory gating properties.
- Dig Deeper! This drug has real possibilities; check out our Tropisetron and Fibromyalgia and Chronic Fatigue Syndrome
Sodium Oxybate
Sodium oxybate (Xyrem) is so unusual the authors put it in a category all its own. Approved for the treatment of narcolepsy, Xyrem is horrendously expensive but targets a key sleep dysfunction in ME/CFS/FM. Two recent studies indicated Xyrem does reduce pain and improve sleep in FM, but the FDA, citing concerns with abuse (it’s been used for ‘date rape’) and side effects, failed to approve it, making unavailable for most in the US.
Flupirtine
A non-opioid, non-NSAID pain reliever, doctors have been using Flupirtine for over twenty years to fight pain in Europe, and it is approved in the US as an anticonvulsant. It’s not clear how Flupirtine does what it does but it appears to involve the NMDA receptors and the sympathetic nervous system. A 201o review suggested Flupirtine may be a unique kind of analgesic agent and interest in the drug has increased recently. A study long, long ago suggested it might be helpful in fibromyalgia but no followup studies were ever done.
Expect Changes
Ablin and Buskila ended the paper on this hopeful note.
“As the fibromyalgia saga continues to unfold, novel and unexpected targets are added to the spectrum of treatments…..Indeed, FMS diagnosis and management in a decade may prove to be very different from what we know today…”Ablin and Buskila
Tried any of these drugs? Tell us how it went. Know of other drug candidates for FM/ME/CFS? Let us know in the comments section.










I tried Xyrem as I have a rare form of narcolepsy where I get no stage 3 sleep along with chronic fatigue syndrome & fibromyalgia. I did not notice that it helped much for FM but am also on Lyrica and other meds for that and other things. Xyrem really affected my gastrointestinal & urinary tract systems causing me to lose 31 lbs (to 89 lbs) and dehydration, urinary pressure, gas, bloating etc which has continued even after going off the Xyrem (never had a problem with either area in 48 years).
Remember, there were only 364 people in the clinical trial for Xyrem before it was rushed through approvals as an orphan drug. As a result, they have no idea of how it interacts with other medications such as antibiotics (which is what did me in) or drugs for unrelated conditions. Xyrem works on the GABA receptors and so will clash with any other medication that does the same. It gave me symptoms simulating narcotics withdrawal when combined with antibiotics and put me in the hospital. Jazz Pharmaceuticals doesn’t want to test Xyrem against these types of drugs as they know there are some really bad interactions. Just remember when you look at the testing results that only 364 people were tested. 1 out of 364 got anorexia – those are actually pretty high percentages when you break them out across a population (percentages for other reactions were higher). Xyrem can be a very good resource but people also need to be careful and vigilant.
Also tried Xyrem after recommendation by my internist who was working on a sleep speciality—he was quite excited about it and thought it would help my CFS. I took it for two weeks—terrible headaches, couldn’t fall asleep on recommended dose so had to double it…it was not a good fit for me and he thought a 2-week trial was sufficient!
Best help for me with FMS/EDS and POTS, to date, is a combination of Tramadol which works on serotonin, dopamine, NMDA and opiate receptors and has a calming effect on my sympathetic system. Along with a Bentyl which is a muscle relaxer and is normally used for IBS – but, it helps all over pain and is great for FMS/EDS. (I told Mayo docs about this combination and they were excited to learn about this combo and the success that I have with it. They said they had not thought to use the two together – but, it would make sense that it would work.)
Alternative things that I use through the day, and works together better than apart, is a combination of Turmeric and Ginger. (Ginger is a warming herb. Helps with nausea but for some can cause the stomach to burn.) Very good for pain and inflammation. Helps to break down substance P and inhibits COX2 expression. Astaxanthin is also great to add for pain and inflammation relief.
I use Turmeric, Ginger and Astaxanthin in the day and Tramadol/Bentyl at night to help with sleep. I also rotate on and off all these things so that the effects keep working. I will come off the RX’s for about 2 weeks and then go back on so that I can keep the dose low and it doesn’t stop working. (Also, eliminates needing to up the meds or cause a dependence issue.) And as with all herbals, you should rotate on and off so that the effects will continue to be effective.
http://www.life-enhancement.com/magazine/article/642-turmeric-may-help-prevent-alzheimers-and-parkinsons-diseases
One thing to note – turmeric can lower NO levels, it is thought —-some feel that it just lowers the free radicals that NO produces and not the NO itself – others feel that it actually lowers NO. For some with POTS there is a need for more NO and not less. I haven’t had any trouble taking turmeric and I feel that I need more NO. (Found out with a rather expensive MCAS reaction that sent me to the hospital. (Interesting side note with turmeric it helps with regulation of histamine release and could potentially be very helpful for MCAS.) This article is a rather lengthy article on turmeric and some of the health benefits that it has. Turmeric is good for so many reasons.
http://www.ncbi.nlm.nih.gov/books/NBK92752/
I did a trial with LDN. I had to come off my Tramadol to try it. I found that it caused me to have pain and severe cramping of my neck and shoulders. It also caused a very bad depression to set in. I was on it for over 2 months and long enough for it to settle out – but, it never did. It for sure helped joint pains and all over body pains, improved sleep. But, the upper body muscle cramps and depression it caused was not tolerable. Since I have a lot of autoimmune issues – I was in high hopes of it working for me. But, it wasn’t a go. That was with a very small amount of LDN too.
Nice article Cort. Few things I won’t be trying – but, nice to know that there is more research out there and more things being looked into.
Issie
I used LDN and actually had no side effects. Proved to lessen pain and anxiety for me. I felt worse at the higher dose level 4.5 and better at the lower dose level of 1.5. Sometimes less is more!
Thanks JD for letting us know….and congratulations on finding something that works. 🙂
Dear Issie,
Thank you for your excellent post.
I am incessantly studying LDN and the dosage and outcome relation.
May I ask you what dosage regimen you utilized.
I sincerely hope that you feel better.
KT
Diagnosis confirmed in January 2011 of FM/ME, I previously learned in 2007, I have restless legs syndrom while be admitted one night in Hospital for potential sleep apnea (confirmed). For now, I don’t have any treatment for rls (all medication make lower pression and then, fainting often) and for FM/ME, I have combination of Nabilone .5 during the day (2mg at night) and if it’s not efficient enough for pain, tramadol take the relay fot eh max of 8 per day. As read before on the website, I try each day to NOT take all is recommended in order to have flexibility in case of higher pain or pain crisis which is frequent. Rhumatologist and neurologist don’t agree on medication and I am a “in between” patient with 2 doctors…But to be honnest, I prefer to follow rhumatologist as he seemed more accurate on FM/ME than the neurologist….
Have you tried first getting your B1 levels up and then adding Alpha Lipoic to see if it helps your restless legs? I’ve heard of several people that this is of great benefit. It also is supposed to be one of the best things for neuropathy. My father was taken off his Gabapentin and told to get Alpha Lipoic for severe neuropathy – as his side effects on the meds was not good.
Issie
Great overview and a more comprehensive list of possibilities. In light of the recent research on immune dysfunction discovered by Behm, et al, Dr. Gillis has told me the FM/a Test is holding water, and there is other research underway that will eventually be published in a peer review journal and the research is not funded by Pharma. While I don’t like to put all my eggs in one basket, I have thought for a very long time there is an immune dysfunction in both FM and CFS and that is a similarity, however, I believe the immune dysfunction is different in each case, just like SLE is different. I hope to see future research that target immune dysfunction and replicated studies.
A long while ago, there was talk of researching a specific NMDA (unlike dextromethoraphan, which is broad-spectrum) combo with opioids, as they have found that when dextromethoraphan is used with opioids in enhances opioid effect requiring lower doses and few side effects. Unfortunately, dextromethoraphan taken in large or continued doses is not good, so they were trying to look at NMDA receptors, target specific.
I also believe that myofascial pain syndrome and the inability to bring it under control when comorbid to FM, is affected by an immune problem making trigger points more difficult to treat in the FM patient. I know they are difficult to treat in interstitial cystitis too, which is considered an autoimmune disorder. That brings us to the prevalence of autoimmune thyroiditis and hypothyroidism too. I just read something somewhere, that hypothyroidism is very prevalent in general and grossly undertreated. Far be it for me to remember where I read that.
I have issues when studies show there is a decrease in pain, but not in function. When medications, regardless if they are psychoactive antidepressants or opioids, lessen the pain because the patient is “gorked out,” it isn’t achieving an optimal goal of improved function so we don’t miss out on important parts of our lives.
I have been looking at the studies on cannibinoids. We are born with specific receptors, and I think that was in the plan all along. I look forward to hearing about the different types and how they work. Unfortunately, the politics of it, just like opioids, is getting in the way. Many FM patients, if not most either completely lack slow wave progression sleep, like myself, or the delta waves of slow wave progression in FM are seriously abnormal. Dr. Harvey Moldofsky is the pioneer on this relationship. While it may not be the cause (I am leaning toward neuro-immune problems), it could be an effect, after all the HPA axis is complex and when it isn’t working right a many things can happen. I would like to see a study of cannibinoids and the affect on sleep function in FM specifically. I think many people stereotype medical cannibinoid users. I will reserve more comments on this when you post your article.
Thanks again Cort, great anaylsis.
A suggestion as to sleep is Lemon Balm. It is very calming to the nervous system and can calm the mind. Some people like Passion Flower – but, it is too strong for me. But, I find Lemon Balm to be a great help. I know one person that uses both.
Issie
Thanks Celeste, and thanks for all the insights, as always…:)
I would stick with Xyrem if it were not for the excessive amount of salt. It caused my BP to go very high. Flupirtine was good for pain, but I had to import it from Germany at a unsustainable cost. Thanks for all of the great work you do.
Thanks John…I had never heard of Flutirpine before….It is licensed to a US company; I hope they can get their act together and find a way to get it into the US…If its works I imagine there’s a great market awaiting them here. ..
Thanks for this great overview, Cort. My head is swimming with all of the possibilities. I don’t know where to start. And I’m nearly doctor phobic after going to so many for so long and having a GP, who I’m afraid to visit for fear he’ll take me off of the things that do seem to help me–Lyrica, clonazepam, carba-dopa/levo-dopa for RLS (brand name Sinemet).
Lina, was Sinemet one of the drugs you tried for RLS?
Sarah, Don’t forget you have control of your medical decisions. I completely understand your fears and have myself been struggling with Doctor care.
Stand up for yourself and tell the Doctor(GP) what has been working and what you would like to stay on.
I wish you strength to advocate for yourself.
I have been taking Xyrem, (sodium oxybate) for seven years. It has been a miracle drug for me and has enabled me to get out of bed, exercise, shop, read, go to college, and have a more satisfying and active life. Before Xyrem I was bedridden for many years, on a high dose of opoids, and in great pain, day and night.
Fortunately, my sleep dr. has been caring for me these 7 years, convinced my insurance to pay the greater part of my prescription, and a charity has been paying my co-pay, as I have lost income. I wish all of my fellow sufferers could have this treatment, it gives me the deep stages 3 and 4 sleep that I can’t get on my own.
My father had this same disease, insomnia, pain, fibromyalgia, for many years. I watched him suffer with no treatments at all. Thank G-d, there is help these days! No more migraines, and my bowels have become more regular. My sleep dr. told me that he treats people with fibromyalgia because we suffer so much more than cancer patients. He is so right, as I’ve had both and still struggle with sjogrens.
SINCE MY friend, ( not) FIBROMYALGIA, has entered my life, I seldom get sleep. I find that if I go to my room, close the door, no pets with a simple cocktail of : Soma ( Watson Brand) ONLY, 200 mg of Tramadol, & 1 (5) mg. Valium, I can get to sleep for a good, good 6++ hours. Day or night this cocktail seems to work 75% of the time.
I have removed the Savella, Cymbalta, LLyrica from any of my med’s. Horrific side effects for me. Mood swings & actually wanting to sleep constantly. Allergies kept me going to the ER with hives & breathing issues with these 3 med’s.
My Pain Dr. has me on Morphine 15 mg. when I can not take the pain any more. I make (1) 30 day supply last as long as 2-3 months. This is good just knowing when you can not take it any longer it is available to take & get into bed.
However, the best medicine that helps 100% is illegal in my state. Marinol/Drabinol , the generic of Marijuana is wonderful. 1 tiny little pill twice a day @ a 10mg does works great.!!!!!
The same CALMING EFFECT. SLEEP COMES EASILY. HOWEVER, THE COST IS Unbelievable.
My co pay on this has gone UP from $178.00 a month to almost $300.00 a month.
I went to every Dr. recommended & finally got the script in my state. Then, the pharmacy made it so high, I can not get it.
They are however the cheapest of all the BIG NAMED Pharmacies.ie: WalMart, Target ,Walgreens, CVS, etc.
Small home town Pharmacies are the best to deal with for their profit margin is FAIR. Target wanted, $1050.00 for 30 Pills. My pharmacy is selling the same pill @ a grand total of just over $ 700.00 for 60 pills. Tell me there is no FIX with our government. Pffft……….
Thanks Emma for all the info. What an eye-opener about Marinnol/Drabinol! I don’t know the prices here in Colorado but it’s much, much cheaper here. I hope your state goes the way of Colorado….It certainly is a great calming and sleep agent…and they actually have energizing strains as well (Wwhich I haven’t tried.)
Good luck with everything.
Hello – I am 57 – had FM all my life- diagnosed at 40. Been using Cymbalta with great results – once the month of bad side-effects was over, and it started working on my brain. Been great with lot less overall pain, and depression. I also have been on Melatonin (5 mg) every night now for 15 years. Great relief – able to fall asleep, and go back to sleep, after the washroom break. Also been smoking pot since I was 13. Great help – able to cope with the general pain, able to nap, able to cope much better being on pot daily. Just wish it was in a capsule form.
I hate to be a downer but I have to say this.
I saw Dr Buskila who wrote this paper. His fibromyalgia research always looks great on paper but in person he is very unsympathetic to his patients and does not know the difference between CFS and Fibromyalgia. He does not recognised ME at all. I have CFS and Fibromyalgia and went to see him. He told me I will never recover if I don’t exercise and suggested that he hospitalise me while I do gradual graded exercise. I complained of my low blood pressure (NMH/POTS?) and he said “Oh just drink coffee. He had no idea of the allergies and intolerances we get. I am intolerant to coffee. I remember crying all the way home after seeing him because he really upset me and took a lot of money too.
His main experience is with patients who only have the tender points/pain but a good amount of energy and who improve with exercise.
I think he is good for those people.
Finally – aren’t a lot of these drugs things that Dr Goldstein used to do with his multi drug approach or are some new?
I am interested in the substance P ones.
Wow….Not a good experience at all….Some of the drugs are new – others are mostly just not on most doctor’s radar. Dr. Goldstein may very well have used some of them but most doctors don’t know about him either…
Sorry to hear about the lousy appointment!
Thanks for your kind reply.
This article you have written from Buskila’s paper is still extremely important and useful. Buskila knows a lot about fibro pain. He is horribly unsympathetic to ME/CFS and post exertional malaise, allergies etc… But Fibromyalgia with pain alone or the dominating symptom is his big speciality.
Therefore this article is very useful if we need to look up drugs for pain symptoms.
Tramadol/Fioricet/Butalbital available zanaflex methocarbamol flexeril are also available for muscle relaxant…. price is very cheap actually prices are at warehouse prices, we have our warehouse at Ventura, CA supplying major pharmacies. I just want to help you guys in regards to financial side while you guys are still on medication,
FYI : We don’t deliver Tramadol to AR, FL, ID, IL, IA, KY, LA, MO, MT, NV, NY, ND, OK, SD, TX & WY as mandated by FDA.
COD via usps priority mail 2-3 days.
I know its hard to get prescription from Doc. We have doctors who will review each and every delivery that we made. Our operation is legit since we follow rules by FDA and DEA.
Feel free to pm me or email me at willowsilos@hotmail.com
I have recently found that Fioricet takes the pain, CFS, brain fog… Almost completely away! This has been a miracle for me, why isn’t this mentioned? It’s in FM forums, just starting to be noticed I guess. This drug is worth a trial!
Fioricet works for me as well. I found this out by accident, mainly because the headaches and nausea were so bad along with fibromyalgia pain. I have great results with this.
I’m brand new here, diagnosed with FM 4 years ago, not currently taking any big pharma drugs specifically for FM after trying gabapentin and gaining 30 pounds in 6 weeks, ballooned like crazy and both my doctors were like, so what? So what if I end up being morbidly obese? How is that going to help my FM? Also tried low dose naltrexone which the nausea side effects were so severe I lost the 30 plus 10 but got to the point that everything tasted really bad and had to stop. I’m not too excited about these drugs and have been researching alternatives low on side effects.
I tried hyperbaric oxygen therapy (HBOT) and my symptoms improved significantly after only 30 minutes worth at a ‘sports recovery’ business. If nothing else, this may be something people could do for special occasions. It really was night and day, like going from a wheelchair to walking again. A friend could not get over how fast I could walk when we got home. There have been studies done showing its effectiveness with FM, TBI, diabetic wound healing, many more, so much so that during one study in Israel, the controls receiving the lower pressure (standing in for placebo) improved so much they stopped that portion of the study and put those folks on the full pressure. It may be that our bodies are oxygen deprived which I have seen mentioned by more than a few people in these blogs. Without enough oxygen, nothing heals is the way I understand it.
Also have read that cortisol levels in FM are not normal which I’m going to run by my PCP next month.
I use memantine, 20mg, and it lowers my pain a lot. No side effects either (the initial side effects, some dizziness, went away after the first weeks).
I can wear most clothes without pain now. Have to take care still, but it works so good.