



I think that this is such big news because it gives proof that this disease is not in peoples heads. I really hope that we can get the word out to patients and even more importantly… the primary care docs and rheumatologists. These studies are “game changers” because they make an incredibly elusive disease tangible and “real”. –Dr. Mark Sivieri
My eyes widened as I looked over at the symptoms this new possible cause of FM/ME/CFS could produce. There it was: burning pain–one of my ‘favorite’ symptoms. More than any other symptom ‘burning pain’ after exercise has been a hallmark for me since I came down with chronic fatigue syndrome over thirty years ago.
There were many more pain symptoms–shooting pain, allodynia, and hyperesthesia, plus many autonomic nervous symptoms. Some ME/CFS/FM docs were finding orthostatic intolerance as well. In fact, one doctor suggested this new finding could, depending on where it was found, possibly account for ALL the symptoms of ME/CFS/FM.
Dr. Teitelbaum had just told me he, Dr. Sivieri, and other physicians in an ME/CFS/FM working group were exploring a new avenue he hoped might particularly help the really hard to treat patients. He and Dr. Sivieri both stressed their results were very preliminary, but both were excited about a possible new cause for fibromyalgia and chronic fatigue syndrome. It is called ‘small fiber neuropathy’ (SFN).
Small Fiber Neuropathy (SFN)
Small fiber neuropathy refers to damage to the small, usually unmyelinated sensory or autonomic nerve fibers running through our skin, peripheral nerves, and organs. These nerves relay sensory information back to the brain and regulate autonomic nervous system functioning.
The symptom presentation is variable–perhaps more variable than doctors know at this point. Nerve-associated symptoms range from feelings of cold, pain, tingling, tearing, buzzing, stabbing, aching, pins and needles, and–what must be a crowd favorite–electric-like shocks lasting several seconds.
SFN can also cause the dreaded allodynia or extreme sensitivity to touch. ‘Sensitivity’, though, is hardly the word to describe a condition in which the touch of clothes can feel like sandpaper rubbing against a wound. On the opposite end of the spectrum, some people with SFN can’t feel anything at all.
Pain just scratches the surface of the possible symptoms SFN can cause. If the autonomic nerves are involved, dry eyes, dry mouth, lightheadedness upon standing, fainting, abnormal sweating, erectile dysfunction, bladder problems, nausea, vomiting, constipation, difficulty with urinary frequency, etc., can all be present.
The damage–which can extend to outright destruction of the nerves–sometimes first occurs at the ends of the longest nerve fibers in the body such as those found at the tips of the fingers (typically the middle fingers) and the toes, but can take place anywhere the nerves are found.
Quality of life scores, not surprisingly, tended to be on the low side–the very low side.
Diseases Associated with Small Fiber Neuropathy
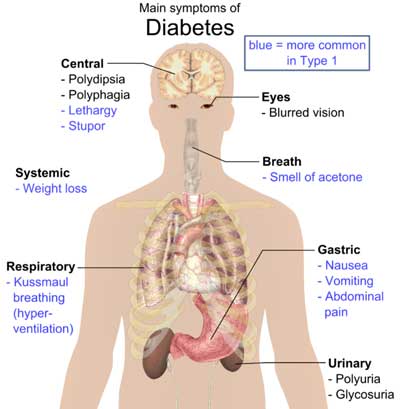
SFN is associated with a wide variety of diseases and disorders including diabetes, thyroid issues, sarcoidosis, vitamin B12 deficiency, HIV, neurotoxic medications (including chemotherapy and antiretroviral agents), celiac disease, Sjogren’s Syndrome, Lupus. With all these disorders, about 50% of SFN diagnoses are ‘idiopathic’; i.e., no discernible cause is found.
Fibromyalgia
“This provides some of the first objective evidence of a mechanism behind some cases of fibromyalgia, and identifying an underlying cause is the first step towards finding better treatments,” Dr Anne Oaklander
No one had looked at the possible association of SFN with chronic widespread pain or the quintessential pain and fatigue disorder – fibromyalgia – until reports surfaced last year at two conferences two months apart. First Dr. Anne Oaklander, a Harvard neurologist, found high rates of SFN in her young, mostly female (73%) ‘chronic widespread pain’ patients. Their symptom presentation; high rates of autonomic nervous system symptoms (cardiovascular (90%), gastrointestinal (82%), urologic (34%)) plus chronic fatigue (83%) and headaches (63%) suggested they might very easily fit the criteria for fibromyalgia or ME/CFS. Interestingly enough, Oaklander also found many experienced ‘reduced sensation’ (68%) as well as pain.
‘Exhaustive investigations’ which came up zero except for high rates of ‘disordered immunity’ (89%) and a family history of autoimmune disorders (33%) suggested she had an immune disorder on her hands.
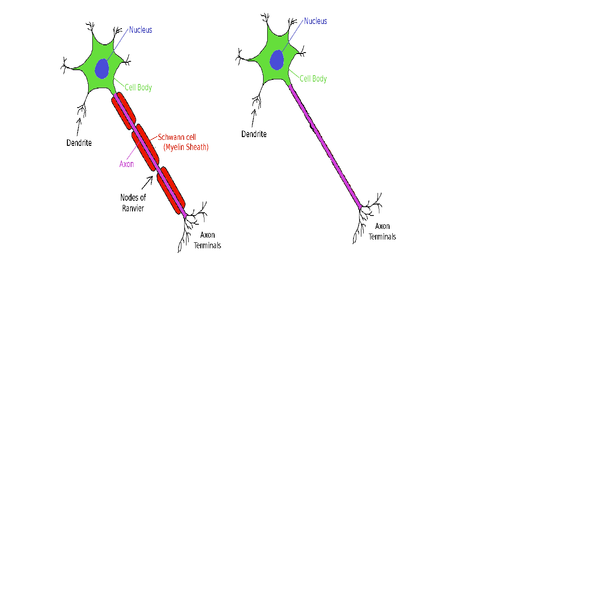
Myelinated nerves on the left, unmyelinated nerves on the right. SFN affects the small unmyelinated nerves
Next Oaklander reported at the American Neurological Association (ANA) 137th Annual Meeting in October, 2012, that almost half of the ‘fibromyalgia’ patients in her study (n=54) had evidence of significant small fiber nerve loss, while none of her age and sex matched controls did.
She believed her findings suggested small nerve fiber problems could be driving the central sensitization found in the disorder.
Oaklander then went hunting for evidence of prediabetes/diabetes–a known risk factor for SFN–and found it in a substantial number of patients, most of whom were not aware they had it. (Her study on SFN and FM was published in June of this year.)
Then in a November 2012 conference of the American College of Rheumatology, Dr. Levine of the University of Arizona reported at that 61% of the 56 FM patients in his study had SFN. The burning, stabbing, tingling, allodynia, and autonomic nervous system symptoms often found in fibromyalgia suggested to him that FM patients might have small fiber neuropathy.
(Notice the interesting possible connections to ME/CFS: the autoimmune disorders, the B vitamin deficiency, the diet connection (celiac disease), the pathogen issues, and the neurotoxic connection; virtually every disorder associated with SFN may have some intersection with chronic fatigue syndrome when all is said and done.)
Fibroneuralgia? ME/CFS/FM Doctors Report
Dr. Teitelbaum and Dr. Sivieri are seeing SFN in two distinct sets of ME/CFS/FM patients: an immune set with high rates of dysautonomia (i.e., POTS, neurally mediated hypotension (NMH), and others) but usually less pain, and a pain subset with little dysautonomia. Dr. Teitelbaum emphasized tests are indicating that the majority of patients with fibromyalgia and neuropathic pain are testing positive for SFN.
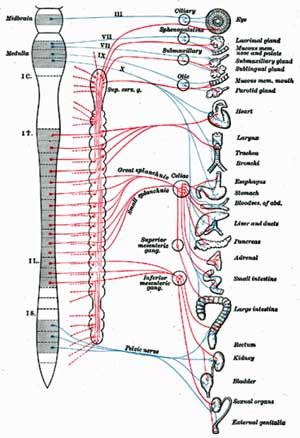
Dr. Sivieri noted SFN’s ability to affect autonomic nerves across the body suggested that theoretically it could
Sivieri’s been seeing ME/CFS/FM patients for about ten years, and he began digging into IgG subclasses about two years ago. Already using IVIG, his ears pricked up when the SFN results began coming in last year. He felt that nerve problems could help explain why a nerve drug like Lyrica works in some people. With these reports coming in suggesting many FM patients have a nerve (and not a muscle) disorder, he suggests fibromyalgia might be better called ‘fibroneuralgia’. It’s still early yet; he’s just begun looking for SFN in his patients, but he hopes the SFN/IgG connection will help unlock the door to diagnosing what he calls an ‘incredibly elusive’ disease.
Dr. Sivieri believes that if tests show you have SFN in your skin you may very well have it in your gut (gastroparesis-like), bladder and genitals (IC and chronic prostatitis and vulvodynia), central nervous system (POTS), and so on.
Postural Orthostatic Tachycardia Syndrome (POTS)
Although postural orthostatic tachycardia syndrome (POTS) (which is a high pulse rate upon standing) was not on that list, POTS and other forms of orthostatic intolerance should be. Teitelbaum and Sivieri are finding SFN in their POTS patients, and a third of POTS patients in one study had evidence of autonomic neuropathy–damage to the autonomic nerves–and decreased sweat output (suggesting damage to small fiber nerves) was present. The increased rates of headache and gastrointestinal problems found in this group could also be associated with SFN.
In the upcoming blog we’ll look at a POTS patient whose diagnosis with SFN eventually led her to a treatment that worked.
Misdiagnoses are Common
Autonomic symptoms can be misdiagnosed as being due to cardiac arrhythmia, colitis or irritable bowel syndrome, chronic bladder infections, skin allergies, or emotional stress.
Given the varied symptoms SFN can cause, it’s not surprising to learn that, like ME/CFS/FM, misdiagnoses are common. In fact, fibromyalgia is on the list of disorders SFN is sometimes misdiagnosed as. SFN has also been misdiagnosed as multiple sclerosis, regional pain syndrome, fibromyalgia, polymyalgia rheumatica, Raynaud Syndrome, restless leg syndrome, IBS, bladder infections, cardiac arrhythmia, anxiety, and depression.
Causes
Small nerve fibers are rather delicate, unmyelinated nerve fibers which can be impacted by many factors. Diabetes most commonly causes SFN but metabolic, immune-mediated (such as autoimmunity) infections, genetics and other factors can cause it as well.
Increased rates of inflammation, reduced blood flow to the tissues and impaired detoxification processes can whack small nerve fibers. Cytokine upregulation, nerve inflammation and autoantibodies appears to contribute to the SFN found in complex regional pain syndrome (CRPS). Bacterial and viral infections (with a nod towards herpesviruses) can hit small nerve fibers hard. Vitamin deficiencies, with a focus on the B vitamins (B-1,. B-6, B-12), interestingly, given recent suggestions low B-1 may play a role in ME/CFS/FM may be involved, can play a role.
In metabolic syndrome high blood pressure and high levels of cholesterol and triglycerides (present in ME/CFS) contribute. Insulin intolerance whacks the small nerve fibers in prediabetes and diabetes. SFN is common in alcoholism as well.
Immune Connection
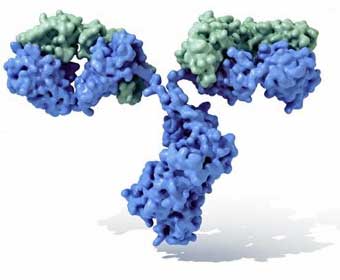
Given the accepted treatment (IVIG) it’s not surprising to find immune dysfunctions showing up. Oaklander found high rates of immune dysfunction (primarily reduced C4 levels) and high rates of autoimmunity (33%) in young chronic widespread pain patients.
Dr. Sivieri is finding high rates of low CD57 counts (Stricker Lyme test) and is consistently seeing IgG subclass 1 and 3 deficiencies. A very early study found reduced rates of IgG subclass 1 and 3 in chronic fatigue syndrome. Immunoglobulins or antibodies are proteins produced by B-cells which neutralize pathogens. Reductions in IgG 1 and IgG 3 often occur together and are associated recurrent infections, particularly lung infections.
Low CD57 counts are often associated with Lyme disease, but Dr. Sivieri believes they may be more a marker of chronic infection and immune dysfunction. There’s no doubt that chronic infections can cause nerve damage; the question for him is whether infection gets so strong that it starts taking out the small nerve fibers in our bodies causing dysautonomia and other ME/CFS/FM symptoms.
Low levels of IgG subclasses only point to a potential problem, and they need to be tied to recurrent infections for insurance companies to pay for IVIG. IgG subclasses play a big role in the immune system memory that allows it to quickly respond to pathogens that pop up again. IgG tests are often used to determine if you’re battling an infection such as Lyme or chronic mononucleosis, for example.
Dr. Sivieri compares low IgG levels to having a jail without cell doors to keep the criminals (pathogens) in. IgG keeps the pathogens (latent viruses) in their cages and low IgG allows the chronic viruses (HHV6, EBV, HSV) and even bacteria (Lyme, Mycoplasma, etc.) and yeast (Candida) to have their way with the body, joints, guts, and brain, and produce a chronic source of pain, inflammation, and immune dysfunction. Dr. Sivieri believes the low IgG subclasses he sees are a big deal indeed.
You’d be hard-pressed right now to find any fibromyalgia guidelines suggesting that IgG subclass testing be done. Dr. Siveiri reported that most physicians will check total IgG levels only when confronted with sinus or recurrent lung infections, and IgG subclass tests are almost never done. His findings suggest that low IgG subclass levels are much more common in patients with chronic fatigue syndrome and fibromyalgia than normally expected. Beyond that, he can’t say much at this point. Dr. Siveri’s and Dr. Oaklander’s findings suggest that this situation should and will change in the future.
Sivieri has a grant to study the low CD57 count (Stricker Lyme test) and IgG subclass 3 deficiency findings he’s seeing.
Because insurance companies will only pay for IVIG based on low IgG levels AND a history of recurrent infections (i.e., chronic ear, sinus, throat infections and/or frequent colds), Dr. Sivieri emphasized these infections need to be meticulously documented by physicians. Patients should provide a timetable or list of the infections they’ve experienced to their doctors.
Autoimmunity, IgG, and Small Fiber Neuropathy
The autoimmune connection with SFN and low IgG levels is a complicated one. Oaklander did find autoimmunity in about one third of her patients, but she found much more evidence of immune dysfunction. Dr. Sivieri explained that the immune system is so active in autoimmunity that high IgG can sometimes be seen.
Essentially we have at least two immune conditions for creating a small fiber neuropathy: an autoimmune state in which the immune system burns out the nerve fibers, and an immune deficient state in which an infection does the same.
Is There a Diabetes Connection?
I have not found an increase in diabetes in CFS/Fibro patients, but I almost NEVER have seen a CFS/Fibro patient that is not sugar sensitive or doesn’t feel much better when they stop eating sugar in all forms. –Dr. Sivieri
Oaklander found a significant percentage of patients with diabetes or pre-diabetes in her cohort. Dr. Kogelnik reported that he’s seeing more diabetes than expected in his ME/CFS/FM patients. Dr. Sivieri, however, stated he doesn’t see a lot of diabetes in his patients, but he thinks something is definitely going on with sugar and ME/CFS/FM.
Dr. Sivieri rarely sees ME/CFS/FM patients who are not sugar-sensitive and believes that sugar, insulin sensitivity, and blood sugar dysregulation can play a large role in these disorders. In fact, he questioned whether any patient consuming a lot of sugar products could ever make a substantial recovery.
He believes it goes further than blood sugar; sugar contributes to the almost universal gut dysbiosis he sees in these disorders. Another good reason to get off sugar (in all its forms (sigh)) is that high blood sugar levels can also permanently damage the very nerves we’re talking about.
Treatment
“These findings suggest that some patients with chronic pain labeled as fibromyalgia have unrecognized SFPN, a distinct disease that can be tested for objectively and sometimes treated definitively,” Dr. Anne Oaklander
Levine was able to find a treatable cause for the SFN in about two-thirds of those testing positive for SFN. Problems with glucose metabolism led the list (n=11), with a significant percentage having vitamin D deficiency (n=5), two having Sjogren’s syndrome, and two with elevated erythrocyte sedimentation rates.
Oaklander reported high ‘improvement’ rates using IVIG in a small study (15 patients). Dr. Sivieri, however, is not finding IVIG to be a useful standalone treatment for fibromyalgia/CFS, particularly in patients who’ve had the disorder(s) for some time. Too much has gone wrong and too much (sleep, diet, pituitary function, brain chemistry) needs to be addressed for IVIG to be a cure-all in his patients. IVIG appears to be working best in ME/CFS/FM patients with low IgG subclasses.
A drug in clinical trials called ARA 20 designed to activate repair mechanisms and reduce inflammation showed some promise in sarcoidosis patients with SFN.
Both Dr. Teitelbaum and Dr. Sivieri emphasized, however, that we’re in early days of learning about the connections between SFN, IgG subclasses, treatment effectiveness, and ME/CFS/FM. Both are investigating the SFN connection in their patients now, and we should know much more by the end of the year.
At a chronic pain conference Dr. Daniel Clauw noted how surprised pain researchers were at the role the immune system plays in producing pain. With several positive FM immune studies recently, a prospective FM diagnostic test based on immune findings, and now this rapidly emerging evidence of an immune mediated nerve problem in FM/ME/CFS, it’s a good bet researchers are going to give the immune system in FM a deeper look. It’s not surprising that he has to start the IVIG lower than recommended and then carefully calibrate the dose with each individual patient. Most insurance companies, however, balk at paying for IVIG more than once every three to four weeks.
Diagnostic Tests
QSART (Quantitative Sudomotor Axon Reflex Test)
An autonomic nervous system test called QSART is most commonly used to diagnose SFN, although it’s more a measure of autonomic functioning than nerve damage. Sivieri does not believe results of QSART tests will be enough to get insurance companies to pay for IVIG.
Therapath
Dr. Sivieri uses a diagnostic services company named Therapath (www.therapath.com) which he described as being very professional and easy to work with.
Video –
The test kits Therapath mails to the doctor need to be refrigerated and have a limited shelf life. They come with tweezers, scissors, the skin punch device, etc., and Therapath provides a teaching video on their website. A 3-mm dermatologic punch is used to extract small skin cores that are examined for nerve fiber density. According to the scientific literature, the sensitivity (78%–92%) and specificity (65%–90%) of skin biopsy tests are good. The biopsy is very small and leaves a very small scar.
Because Therapath has control data for only three locations on the legs, the biopsies must be done in those areas for pathologists to certify a positive test. It is interesting that the biopsies are not done in areas where people with fibromyalgia feel much pain.
Insurance companies usually pay a significant portion of the costs.
Conclusions
“The next step of independent confirmation of our findings from other laboratories is already happening, and we also need to follow those patients who didn’t meet SFPN criteria to see if we can find other causes. Helping any of these people receive definitive diagnoses and better treatment would be a great accomplishment.” Dr. Anne Oaklander
It’s very early yet but small fiber neuropathy has the potential to present an entirely new way of looking at fibromyalgia and chronic fatigue syndrome. Well accepted and easily diagnosable, (at least in the skin), SFN may present a new pathway to legitimization for both these disorders. With the possibility that multiple system involvement could produce a wide range of pain and autonomic symptoms, SFN could be made to order for symptom-rich disorders such as ME/CFS and FM.
Dr. Oaklander cited high success rates with IVIG that may or may not translate to ME/CFS or FM. Citing expense, Dr. Teitelbaum has eschewed IVIG, for years but now holds out hope it may help his more severely ill patients. With some miracle cures and mostly moderate results, Dr. Sivieri sees IVIG as one tool that needs to be supplemented with others to be successful.
With just one published study, two conference reports and a host of anecdotal findings we’re still very early in the SFN saga. The next year will tell us much.
(Thanks to Dr. Teitelbaum and Dr. Sivieri for their help. All errors are mine)













GREAT WRITE UP, Cort.
You told me you had a big one coming up and I’d like it. For sure! This has been the findings with many of us. I do have low IgG levels and IVIG was suggested to me. However, I’m working on my immune system in a different direction –
One thing about the autoimmune dysfunction, there are 5 classes of immunoglobulins that are checked, IgA, IgM, IgE, IgD IgG and three different subsets of IgG.
http://www.wellness.com/reference/allergies/antibody-deficiencies
IVIG carries warnings the same as a blood transfusion. It is antibodies donated from many donors. I’m using the Immune Formula of Symbiotics brand of Colostrum. It can give antibodies and doesn’t have the potential side effects. There are other things that I’m also doing for my immune system (diet, low dose antibiotics, low dose antimalarial herbs, anti-inflammation herbs, Vit D, C, B1, enzymes, probiotics and others).
___________________________________________
http://www.advocacyf…hat_is_ivig.pdf
18. What is a alternative to IVIg?
If you cannot get IVIg there are alternatives available, colostrum is a natural product which also contains IgG and antibodies, the best colostrum would be freshly obtained liquid. Weaker forms will be the powder forms.
_____________________________________________
It’s exciting that so many doctors are starting to recognize the immune connections and treating us accordingly. I do feel this is the key to our wellness. Inflammation is a close second.
There’s so much more I could write about this. As it’s exciting to me to have figured this out. And I want to shout it to the world. Of course, when I start to learn about something, I really dig into it wanting to understand the WHY of things. (It’s been a great learning experience.)
There are for sure things we can do ourselves. Even if the doctors haven’t discovered these things in us yet. If we feel there is a problem; we can work on the things that would address it, ourselves, and that can even be more diagnostic and define things even more clearly.
The end line of it all, even if there is SFN, is the immune system is not reacting properly. Attacking what it should not, and letting go things it should attack. We need to get that system working properly and we’d all be better. And yes, this can affect all the illnesses that we are talking about and I’d venture to say – could be the underlying factor. 🙂
Issie
Thanks for the tip on the colostrum…Interesting that you have low IgG levels.
I agree – SFN is the symptom not the cause; hopefully if these findings do work out it’ll lead to more research and get us closer to the cause – at least for a subset of patients.
Thanks for all the info. 🙂
Issie,
I am new here, just finding this site today and have spent the whole day reading. I have found so many answers and explanations to so many things that even my doctor could not answer. He tries but is failing me in so many areas. I would love to discuss with you your more non-pharmaceutical approach as the pharmaceuticals are causing me more problems than I had to start with and with my many allergies some just aren’t a possibility. If you would be willing to discuss this more, please let me know. If not, that is perfectly okay as well. Thanks to you and everyone else here. You are all educating me so much!
How do we become part of this. I’ve got low OGG and theee subclasses
great piece. You assimilate seemingly disparate facts like no one else.
Up pops the autonomic system again, eh? Possibly with connection to the immune system?
Unfortunately, I have not heard of much clinical success with small fiber neuropathy patients…. I would be thrilled if somebody could point out some successes. My guess is that the small fiber neuropathy is, if anything, representative of the underlying issues in the immune system and autonomic system. But that’s just a guess.
thx for the post…
I also feel my CFS started with such extreme stress and that my ANS is key to whatever will heal me. I am sure I also have the SFN, but not as the cause. God, if I could just calm down my sympathetic nervous system and get some SLEEP! I don’t ever know where to turn at this point. I was part of Dr. T’s clinic process, but all it did was cost me about $8000 that I could not work off “after I got well”, because that never happened. I love Dr. T. though and feel he is totally honest and sincere. I had a good doc at the clinic too. But they never looked at my ANS and after all I have now read, I am sure that is the key for me.
Joya, I’ve found that Lemon Balm calms my system down and helps with sleep – it works on increasing GABA – which is calming. My sister also uses Passion Flower with it. For the tachy that goes along with POTS and that jump out of your skin feeling –Motherwort calms that down in about 20 minutes. I’ve also found that Black Strap Molasses is calming to the system – it’s high in potassium and iron.
Colostrum is also calming to the nervous system but at the same time gives energy. You are supposed to not take it too late in the day, because of that.
As for neuropathy, I’m getting better. There appears to be a genetic/autoimmune form in my family. I’m starting to get the feeling back in my legs and feet. I can feel the little bumps in the bottom of my Crocs (yes, I like them – even if they are not the most attractive 🙂 ) It’s really amazing how much improved I am in the last 7 months. There is hope!
Issie
Thanks so much, Issie. Your thoughtfulness is very much appreciated. I really appreciate finally finding others who understand and don’t think I’m making it up, or whatever it is they think. I am very happy to be reminded of colostrum. It cured my CFS induced mononucleosis years ago. A good investment and doable. Thanks again, dear Issie. joya
You’re welcome. Let me know if some of it makes a difference. Hang Tight!
Issie
I’m looking forward to trying colostrum as well…Thanks for highlighting that 🙂
Hi Joya,
I have found a product that works very well for my sleep issue. It’s a natural product, Anavone from Maxam Labs. Also very helpful with stress response. It’s an adrenal gland support and their probiotic formula, PHP, is the best I’ve tried. I also take 1 TBS of a powder magnesium supplement at night. Between those 2 and with the recent addition of B1, I am sleeping through the night.
http://www.maxamlabs.com/
Oaklander did have some success with that small sample. Teitelbaum apparently has had some success with some of his really ill patients and Sivieri has had some ‘miracle cures’ but I agree that this is just a start. If the finding holds it will definitely put more emphasis on IVIG – and that will surely help some people who haven’t tried that yet – but my hope is that it leads to more research.
Lots of things can cause SFN – that’s a little disappointing 🙂 but finding it should really help legitimize both ME/CFS and FM. I hope the studies work out…I would be surprised if they didn’t but we’ll see.
One thing Dr. Teitelbaum wanted was to get the message out so that more doctors check it out.
I thought that SFN is supposed to apply to the small fibers in the skin of the extremities. Is it generally accepted that non-myelinated small fibers are all over the place and that this condition can affect so many aspects of the body, the autonomic nervous system, digestive tract, etc.? Is this accepted knowledge?
I was diagnosed with SFN a few years ago by the punch biopsy test and am also considered to have Pandysautonomia–in other words, many autonomic nervous system problems. My surface area is quite numb in some areas and in other ways hypersensitive. From the jist of this article, all these issues could be related to damage to the non-myelinated fiber network?
It would be useful to have a list of all the possible ways that SFN can manifest in the body. I also want to know what the future will bring. How bad will this get? Does it stabilize or is it always progressive and to what end?
Cecelia,
Maybe somebody else can come up with something better, but there is a forum called “neurotalk”. I’m not sure if you’re familiar with it or not…. Within it, there is a sub- forum entitled “peripheral neuropathy”. There are some People active in that sub forum that are pretty knowledgeable about small fiber neuropathy. It is a extremely complex subject.
You have any success treating it?
Tim, do you know how to get in touch with Rich? He is on another forum on Facebook and has done a whole lot of research on SFN. He has connected it to his breathing problems and would probably have his research available. He is really talking about what he has learned in its connection to POTS. I don’t know what site he is on, as he hasn’t been on DINET in awhile. He’d love this conversation!
Issie
Sadly Rich died last year.
Different Rich. This is a guy that has POTS and was on the DINET forum for awhile and went to Facebook. Sorry for the confusion. I thought about that after I posted my question that others would get confused. (I actually got in touch with the guy I was wondering about.) I’m sure that the Rich that died would have enjoyed these conversations too. His search for answers is over. He is in a restful state and is no longer suffering. That’s what we all wish for. The people left behind are the ones that suffer —we miss them desperately. But, they are no longer in pain. We can take comfort in knowing that. Sorry, for the confusion and causing others to remember their friend whom they miss —but, hopefully that remembrance is with great fondness.
Issie
My understanding is that yes, it is accepted knowledge that these nerve fibers are found all over the body and could be affected in many places.
Oaklander found high rates of pain and high rates of desensitization in her patients, so I assume – yes, you can have both :)…How fun is that, huh?
I’ll be digging deeper into SFN…I have no idea about prognosis at this point.
Mayhaps I’m reading this wrong (imagine that!) but I see a good many contradictions in this research summary. This is an article that I’m NOT comfortable handing over to any physician. I realize that it’s just a one study and just a starter theory, I’m not gonna bet my few pennies that this will pan out. Of course, I’d love to lose this bet.
Me? I’m heading for the icHHV6 labwork as my brother has MS and my daughter Raynaud’s. I’ve already got an RX for Valcyte but I’m hesitating to take it until I get this particular labwork done. As well, I need to read up on the side effects and dangers of Valcyte. I took Valtrex for years with no problems. It did seem to help my lowgrade fever recede but that was about it.
I am curious if any of you have been found to have stenosis (calcification) WITHIN THE INTERIOR of your vertebrae. After 10 years on Methadone for pain and the pain being primarily a feeling that a truck had run over both of my arms, especially the left one, and a diagnosis of FM, it was finally discovered that I had 2 severely herniated cervical discs that were taking my spinal cord with them. In January 2012 I had the discs removed, spacers put in that were to eventually make solid bone from the arthritic bone spurs they’d tossed in, and a Titanium plate screwed into the side of the vertebra to hold it all in place. My luck, this didn’t take the pain away so a second MRI was done and they saw that the interior of those vertebra has calcified (stenosed) and were consequently squeezing on my spinal cord. August 2012 I had second neurosurgery but they sliced the entire back of my neck open this time to better access the interior. A couple of days ago I hit my one year post-op anniversary of this surgery. The result? A trade-off. While my arms no longer hurt as bad (feeling like a truck ran over them was not an exaggeration), I now have basically my entire neck fused together and a Titanium plate on each side. That means I have to lie on the floor if I want to look at fans to purchase, on the ground if I want to look at the stars, step on a stool if I’d wanna hug Cort since I’m 5’1″ (or not look up at him), and many otherwise normal activities still leave me with neck pain. But at least this pain is REAL and not one that felt like it was coming from my brain and that my arms were going to explode from the inside out. I now take 10mg hydrocodone when needed and am forever thankful to the pain MD at Augusta Back for being so empathetic.
Lastly, I’d like to encourage all of you to make sure that your MD isn’t simply testing your TSH levels as is still common practice. CFS/ME cause HPA axis suppression and your doc will need to check your free T3 and T4 levels to ascertain whether your body has enough thyroid hormone. I have been taking Armour thyroid 45 mg which is made from pig thyroid (dessicated). SYNTHROID DOES NOT WORK!!!. I did recently read about a compounded natural thyroid that works better than Armour but thus far my blood levels are normal. If you have thinning hair, mayhaps a bald spot in the front, lacking the outer third of your eyebrows, a low basal body temp, and/or very dry skin that you don’t remember having previously, weight gain for no good reason….these are but a few signs of low thyroid, hypothyroidism. I only got on the correct dose just before my January 2012 surgery and while I have lost a LOT of muscle mass to be accounted for, I’m nonetheless down from about 140lbs to 117. Now I don’t eat right or much but I’ve NEVER eaten right since I live alone and CFS became my life so it’s difficult to account in any exact way for the weight loss. And I DON’T want to lose any more. Hanging skin looks worse than well-rounded sensual skin. That is something I never in my life thought I’d say…. Anyway, that’s my crash course on Hypothalamus-Pituitary-Adrenal Axis suppression which creates not the usual primary hypothroidism but a SECONDARY one. Good luck with your docs. Ain’t it wonderful to find one that’ll let you bring in an article and cooperate with your testing requests?
Now we need to work on getting more doctors educated since CFS/ME is not even taught in medical schools yet. I spoke on the phone with Dr.Elizabeth Unger who is in charge of the chronic illnesses part of the CDC. She stated they are working on beta testing small groups of medical students but the final curriculum (hopefully ready this Fall) will need to be approved by the American Association of Medical Universities. Continuing Education Units (m.e.u.’s) ARE ALREADY AVAILABLE on the CDC website for practicing MD’s, another fact she told me that I was completely unaware of but admittedly have yet to look at myself. Hang in and keep fighting however u can.
I realize that none of you…. that I’m new to the comment group. But I’ve had CFS diagnosed since 1994, had to quit my nursing career in 1999, tossed out by my family in 2000, and have lived alone since. REALLY alone since Zeus, my bestest friend black lab left me at age 14 on February 15. Anybody live near Bountiful, Utah so that I can get one of his relatives? Anyway, I’ve been a member of the CFIDS Association of America since science was blaming CFS on chiari malformations and while it was considered a psychiatric diagnosis. I’ve stayed up with the literature, written many letters to many people (and I do not mince words), and most recently testified via phone to the CSFAC in May 2013. I was scheduled for the day prior but just could not do it and they kindly allowed me to speak on day 2 at about 3:15. My current goal came from my realization that the medical teaching university in Augusta, GA, it’s hospital and clinics…. that not a single MD knew a single fact about CFS/ME. Their Family Medicine Clinic consists of at least 20 MD’s, many professors who teach at the Medical College of Georgia as it’s all together. It blew me away to think that people go to a teaching hospital/clinics presuming they’d get the newest and best care but yet anyone with ME/CFS would most assuredly leave without a diagnosis, thus assuring that their Social Security app would be turned down. As well, my first FM doc got so flustered with his ignorance that his idea of revenge was to send me to every specialty known. That’s when I realized that CFS/ME DOES NOT FALL UNDER ANY SPECIALTY’S “SCOPE OF PRACTICE” (not my area, lady) meaning they have no protocols to follow. PROTOCOLS are everything to an MD. Kinda like”if this, then that” flow of directions to follow. Without them, they are rendered impotent and perhaps even accountable legally for screwing up a recipe they’d concocted on their own. Herein lies the real problem and this is what needs to be dealt with before CFS/ME EVER gains the legitimacy we continue to complain about. OK. I know I’m way too verbose but I hope that if anyone reads this they’ll find my point valid. Like, I’m being paid SS Disability for an illness with an ICD code that belongs to no specialty and that no Primary Care MD knows squat about. Wonder how the Federal Government would feel about that?? Anyway… tell Cort to fix it. Kidding, dude. Sorta. Marcie
Marcie, I’m sorry to hear about Zeus. I understand about feeling alone with this illness, though you seem much more connected than I am able to be. Are you aware of or have you found benefit from connecting with O.F.F.E.R. The Organization for Fatigue and Fibromyalgia Education and Research (offerutah.org), centered in Salt Lake City? They hold monthly education/group discussions at the Salt Lake City/County building 7 p.m. the first Wednesday of each month, and load the video of the discussion on the site.
I wish all the ‘technical’ talk wouldn’t be flying so far over my head…
I have had CFS for 30 years. Just started getting the burning and tingling and numbing of Small Fiber 5 years ago. Would SFN also cause swollen glands, flu-like illness, extreme fatigue? you may have covered this in this article, but I do have the flu right now and couldn’t read it all. For now, it sure is a wait and see.
Agreed that these findings have the potential to be a ‘game changer’ but only if taken forward logically.
As already noted peripheral neuropathy is associated with a number of conditions ranging from autoimmune diseases to ‘self induced’ chronic alcohol abuse.
Does it makes sense to rush into IVIG treatment on the basis that it might be useful in a sub-set of patients? Wouldn’t partial success just muddy the waters.
Plus how does peripheral neuropathy relate to other symptoms such as ‘fatigue’ and cognitive problems? Do patients with peripheral neuropathy also have autonomic neuropathy? What about those patients who don’t meet the diagnostic requirements for PN – does PN play no role in their condition or have they just not reached that stage yet.
Better in my view to replicate these findings (and autonomic dysfunction) in a large sample and then try to work out what is the pathology underlying PN in all of these conditions which is also then likely to apply to fibro/ME/CFS.
As previously blogged, the most consistent findings in ME/CFS are raised levels of the pro-inflammatory cytokines IL1b, IL6 and TNF-a (TNK-a induces release of the other two). So what? These are not specific findings and similar patterns are seen in, for example, major depressive disorder, diabetes, chronic alcoholism etc. Well, that’s just the point!
Julia Newton’s team are currently working on primary biliary cirrhosis as a model for fatigue in ME/CFS. Recent findings suggest that polymorphisms in a TNF-a modulating gene may mediate ‘sickness behaviour’ (fatigue, mood, malaise) in PBC patients. It probably wouldn’t surprise you to learn that autonomic dysfunction and peripheral neuropathy are commonly found in PBC.
You may also not be surprised to learn that drugs that block TNF-a have been shown to ameliorate PN in animal models : http://www.ncbi.nlm.nih.gov/pubmed/23735240 and are currently under trial for PN in (human) diabetes patients. http://www.slideshare.net/brianwells/the-effect-of-tnf-blockage-on-diabetic-neuropathy
TNF-a’s impact on the clearance of extracellular glutamate makes it a prime candidate for neurotoxicity both in the brain and peripherally and could well explain the occurrence of both autonomic and peripheral neuropathy/neuropathic pain – and hence all our symptoms.
I’m actually more interested in Fluge/Mella’s experiences with TNF-a blocking Etanercept than in the Rituximab trial.
So, what it all boils down to is predisposed genetics, with autoimmune dysfunction and inflammation. We have to get to the core and the “peripheral” things (play on words) will come into check. 🙂 We can research neuropathies and myopathies and all the different forms of each and the possible reasons for them developing —-but, ultimately —it still will come down to those three things. Now whether or not we can “tweak” those things, activate or deactivate – depending on the direction we want them to go —who knows. Will we only be able to “mask” the symptoms with a “purple bandaid”, or can we eliminate the problem? That remains to be seen.
Side note —in Chinese medicine, issues with the liver also bring about anger issues. So, for sure a dysfunction with it can be mood altering. Some are finding that there is a dysfunction with the P450 pathway and the detox ability of the liver. This would also affect how we metabolize medicines and herbals. Could cause a build up of those and that could be one reason why a person is super sensitive to certain things, and require less. As instead of it being eliminated, it may be recirculating in the body.
Issie
I agree! The key here is to validate these findings – get them legitimized in whatever group they’re present in and then get the funds to go searching. The key is getting the funding to dig deeper. Then who knows what will show up? Insulin problems in some prediabetics, herpesvirus infections in others, gut caused inflammation in others?
The fact that inflammation is present may be the key; aka those intriguing TNF-a findings in PBC…
Marco, you’re going to love this article:
http://www.ncbi.nlm.nih.gov/pubmed/23726157
Autonomic diabetic neuropathy is evident in individuals that experience a long-standing diabetic disease state, and gastrointestinal (GI) dysmotility is thought to be the outcome of neuropathies within the enteric nervous system (ENS) of these patients
a diet independent, age-associated decline in glial cell populations. This is the first study showing that mucosal glia cell damage occurs during diabetic symptoms, suggesting that mucosal enteric glia injury may have a pathophysiological significance during this disease
__________________________________________________________
This is the part I like —because it’s showing that a high fat diet – they think contributed to this:
___________________________________________________________
The high-fat diet caused obesity, hyperglycemia and insulin resistance after 4weeks. These changes were associated with a significant decline in the area density indices of mucosa-associated glial cell networks,
________________________________________
How much would a diet change accomplish? Low-fat, whole food, vegan, is making a difference for me.
Issie
Can damage to these small fibres heal naturally over time, if the cause is eliminated?
The nerves can heal; Oaklander and Sivieri found that IVIG reversed the problem in some patients. My laymen’s guess is that IVIG got what pathogen was the problem under control and that reduced the inflammation and the nerves healed.
IVIG increases the antibodies levels in the immune system to detect and fight whatever it needs to (pathogens, virus). It’s IgG (immunoglobulin) that a person may not have or is not producing in their own bodies. So, it would help the autoimmune system to work better. (Colosturm is supposed to be an alternative to this. Without the risk involved.)
http://bdipharma.com/Clinical-What-is-IVIG.aspx
Issie
Bbnormal activity i.e. upregulation of the autonomic nervous system is the key driver of this disease for most patients. All signs and symptoms can be explained also those of the immune system.
Abnormal…
bbnormal or abbey-normal? 🙂
Chronic upregulation of the SNS can have profound effects on the immune system including pushing towards a Th2 state. You may be right…
I respectfully submit, these studies that look at damaged tissue, are exactly what one would expect to find when there is pain and numbness. I believe it is just as obvious that a TOXIN is the cause, in the absence of a Pathogen.
Hematology, we can’t discern what the Toxin is and where it came from?
What we do know, is that we all have biofilms. Biofilms surround like a force field or protective field around virus, bacteria and pathogens. If we can get the biofilms to break down and the immune system and/or whatever aid we are using (antibiotics, herbals etc.) to be able to gain access to the things causing the problem – and either eliminate or control the growth of these things. We should get better. We may not can totally eliminate the problem. But, I’m sure we would all welcome “Better”. However, slight that may be.
One of my friends hypothesis is that SFN causes an imbalance in the autonomic system. But, what caused the SFN and the autonomic system dysfunction? (I think my friends way of thinking about it is considering the result not the cause. And it’s a big circle of what came first.) Ultimately, wouldn’t dysfunction of the regulation of the autoimmune system and/or imbalances in certain hormones cause SNS dysfunction? And, that could contribute to autonomic nervous system disorders. But, could autonomic nervous system disorders also be a result of improper immune system function? I think this needs to be explored more.
One thing we can do if there are autoimmune issues is see if Colostrum makes a difference. Since it’s an alternative to IVIG. There are other things that can be tried to. Things to eliminate pathogens, bacteria etc. (Silver, probiotics, olive leaf). Things that can tweak TNF and help with inflammation (turmeric ginger, astaxanthin). There’s things we can do. The biggie, and the one thing people seem to not want to change or tackle, is our diet. That can affect the immune system and could change/correct so many possible issues. Then there is also looking at mutations with genetics and possible “tweaks” with epigenetics; and diet also plays a big role in that. Our diet could be one thing contributing to many genetic changes that could be inherited and passed down generation to generation. It’s the one thing we learn from our families and that is a continued pattern – possible keeping the dysfunction alive and on going. There are things we can do. Looking for the perfect medicine without making lifestyle changes – will only mask the “core” issue. We need to do what we can to change things. We have to take responsibility for our own health. We do have control over the things we do. It’s up to us to not look to someone else to “fix” it. We can do a lot of positive things ourselves. And then when those things are in place, look at what’s left over, and find the “purple bandaid” for those things. We won’t have the need for so many bandaids — and that will be the best we can do for ourselves. Keep a positive attitude and do whatever you can to improve your life situation. Take control of it. Don’t let “IT” take control of you.
Issie
I just got this sent to me and it so much lets me know this is a part of the problems. It’s not long, please watch and consider it.
http://drmcdougall.com/stars/roberta.htm
Issie
This is NOT NEW! I posted this article all over various FB sites to give
people hope, then I found an old study from 2008 done at UCLA
http://www.ncbi.nlm.nih.gov/pubmed/18208823. Here is a response I got back
from someone who may have had the hopes raised when they saw the post of the article above:
“IVIG has been used by people with CFS and ME for a long time. Sadly, it didn’t
help me”.
I feel really bad that I advertised this as new to people 🙁 Guess I really
need to research my sources better. Cort, were you aware of the 2008 study?
Do you know if there are any other studies from back then? The
Massachusetts study even touts this as new. I guess they’re advertising for
themselves.
Anna (feeling like an ass)
Sorry you feel bad 🙂 I was not aware of that FM study but there are also a few IVIG studies in ME/CFS that got differing results. A Korean doctor has reported great success with IVIG at ME/CFS Conferences.
IVIG is not new… however, it’s not commonly used in either of these disorders and few doctors look for IgG subclass deficiencies or for small fiber neuropathies… The really new finding,for me, is the small fiber neuropathy. Is it really present alot in ME/CFS? If it is then we have an opening that may be able to explain alot of the symptoms in ME/CFS (legitimize the disorder) and push research in that area.
The treatment end – IVIG for the most part, is not so exciting at present but it does present possibilities for the many patients who haven’t tried it. A upcoming blog is going to highlight someone who did very well on IVIG…
So, yes IVIG is not new – particularly to patients who’ve tried everything…but it is surely new to many others…:)
I have low igg level sub class 1-4 and I would love to be a part of this study. I have gotten ivig in the past and it made me feel better but it was hard for me after the first day of treatment my body was trying to reject it. I did the treatments for 2 years till I lost my insurance and now have been told I have fybromaliga Can someone contact me if I can be apart of the research. Thanks
There is another research study to determine if peripheral neuropathology causes Fibromyalgia pain, intolerance to temperature variance by Dr. Rich. This research is different and is not to be confused with Oaklander’s. research.
http://forums.phoenixrising.me/index.php?threads/fibromyalgia-rational-biological-source-of-pain-found.23868/
https://www.ncbi.nlm.nih.gov/pubmed/23691965
I found this information interesting. As I question if there is some sort of issues with the valves of the body in regards to blood flow with POTS patients. This could also explain some of the problems associated with that. I know with me, the cold for sure is not a good thing. But, extreme heat isn’t either. We know that temperature plays a part in vasodilation and vasoconstriction of the veins. Those of us with POTS can’t take a hot shower as it will make us become severely symptomatic. But, being really cold, makes some hurt terribly. Most POTS people can’t take extremes in either direction. There is a fine line in what is tolerable. Many POTS people, because of the autonomic nervous system malfunction, have to wear cooling vest in the summer because the body doesn’t regulate temperature properly. Some don’t sweat and can’t internally cool their bodies down when overly hot. (Symptoms similar to MS.) But, get overly cold and the pain is horrible, at least it is for me.
I just love the fact that there are really interesting ideas out there that are being pursued. Lots of positive steps in the right direction.
Issie
Dr. Teitelbaum introduced me to SFN and he commented on the blog and the recent findings on Facebook;
“Thank you Cort for another excellent article! TO put this in perspective, it :1- is another part of the puzzle, augmenting the role of nerve pain occuring in response to both chronic pain and immune dysfunction and (2)- This treatment is not needed for everyone, with the IVIG being very expensive, but is showing benefits in that 10-15% of people with the most severe CFS/FMS, who are often bedridden/housebound, and that have marked immune and autonomic dysfunction, and have poor/inadequate response to other treatments–making it an important step forward for that subgroup!”
I am so bad off..just want to see enough evidence of physiological manifestations so that medical “institutions” and insurance companies cannot deny us our known realities…that we are suffering from something that is attacking our systems similiar to lupus or any other immune disease or in some of us virus’s that act like non hiv aids..I’ve seen recent research that shows that gut disfunction is tied to austism, which has been tied to vaccinations…demyelination of nerves have been tied to many diseases, some of them mentioned in this article..one of the big ones is MS…demyelination is one side effect of vaccinations…it can be found on the vaccine inserts…more and more research is pointing to disregulation of many of our systems..we can do the science all day long, finding the “whys” of all of this..but what is the fundamental “why”, the trigger of all of this?…vaccines have been found to trigger autism, cancer, diabetes, MS, many immune disfunctions..we have recently seen on the CDC website where they admitted that polio vaccines contained cancer cells..of course that confessional piece was quickly taken down..as long as monies for research come from or the research is done by government institutions, it appears that no amount of research will be allowed to tie vaccinations to any of this no matter how overwhelming it ends up being..even if it does those research papers would never be allowed to published in any mainstream publications, because no mainstream research will be done and that is the only type of research work allowed..it’s an endless catch 22..so instead of accepting that vaccines are fundamentally unsafe, and doing the research to find better alternatives, the “public” is left to mop up the mess. Trying to find the better drug that will ameliorate all of this damage, which, in turn, will make even more money for the pharamceutical companies, those same industry folks who brought us those horribly damaging and in some, death producing, vaccines is dishearting. But for those that already have the damage it give us a bit of hope that we might find some relief from our suffering…before I got “sick” my brain was able to function so much better..I think I could have brought something more “scientifically” based to the table..now I just have my own opinions…
Does anyone have experience with polymorphisms/mutations in the sodium channels in nerve fibers (esp Nav1.7 and Nav1.8) and familial or sporaic fibromyalgia? Particlarly with autonomic dysfunction? Greg
Hi, nice blog. I think SFN explains something that has been going on with me for over a decade. I was diagnosed with Trigeminal Neuralgia by a GP. But it spread throughout my body as I got more ill about 2 1/2 years ago with my GI system in particular. My symptoms are a type of stabbing pain in my head, followed up by “neuralgia” type pains in my face, gums, around my eyes. These were symptoms from a decade ago. Then a couple and a half years ago got worse. About one and a half years ago I had these sort of pains come in a new area in a stocking fashion from feet and hands to torso. So now I can get the pains anywhere but in particular have burning and pin prick sensations in hands and feet, and nerve type soreness in my scalp, face and mouth…also get a burning tingling tongue. I got diagnosed with UCTD a year ago…not yet treated I am now under further investigation for my gut which is really bad in different ways…GI doc metioned over sensitivity?…but have bad reflux symptoms, swallowing pain, etc. Got joint pains, muscle pains, etc [the UCTD]. Wondering if I might have Celiac Sprue and Lupus causing this in me. Seem to have developed a sudden intolerance to milk after going gluten free…have still got digestion issues. I also suspect Ig subclass abnormalities as being quite likely with myelf because my IgA tested on the low side [overseas test]….but I doubt the NHS will look at this.
Thinking of trying Colostrum also to try and set Igs astraight but waiting to get fully diagnosed first. Thinking of trying camel’s milk also. Camel’s milk is supposed to be full of unique immunoglobulins which are believed to act to block out auto-antibodies. …though would most likely need to be avoided by anyone with folate receptor antibodies [check with a well qualified Dr in this regard]: http://nourishinghope.com/2011/11/camel-milk-healing-or-hype/
Some herbs that might be of benefit in auto-immune disease…though check with your Drs first……there are known [and implied unknown ] herb drug interactions with some drugs and some herbs. Here is an interesting article on some herbs that might be of benefit:
Natural Support for Autoimmune and Inflammatory Disease…posted by Journal of Restorative Medicine on April 1st, 2013 in Journal by Eugene R. Zampieron, ND, Ellen J. Kamhi. , PhD, RN ©2012, Eugene Zampieron: http://restorativemedicine.org/tag/artemisia-artemisia-annua-qinghao/
Is Multiple Sclerosis related to this?
Yes Sfn plays a big role in pots – a third have abnormal Qsart and importantly another 20% had abnormal MIBG reupatke in the cardiac muscle suggesting cardiac sympathetic denervation.
A recent study of pots patients found that a large percentage had simple autoantibodies to alpha 1 adrenoceptors blocking the action of norepinephrine.
In sudden onset waxing and waning Sfn the primary pathophysiology is almost certainly autoimmune or cytokine driven auto inflammation.
I encourage anyone with pots fibro and Cfs to get a Qsart test or skin punch biopsy. Partiularly if they experience increased or reduced sweating, weird changes to temperature detection in feet or mottled skin (you cort!)
If its cytokine driven it might prove quite easy to treat.
Thanks Gibbo:)
Just some clarifications:
a peripheral neuropathy is quite different to small fiber neuropathy. Peripheral neuropathies usually refer to damage (often permanent) to the large nerves of that hands and feet. Small fiber neuropathies can present peripherally first but have been shown to appear almost anywhere in the body – cutaneously, splanchnic even on the scalp.
another important point is that in general small fibers can repair themselves.
there are studies that demonstrate in Sarcoidosis that Pots with abnormal small fibers responded completely to TFN alpha inhibition – so that the patient went into complete temissionsuggesting cytokine inflammatory damage rather than autoimmunity at least in this case.
There are literally hundreds of patients on Facebook with pots and abnormal QSART that are responding to IVIG.
destruction of small fibers theoretically could result in abnormal input into the central nervous system resulting in compensatory up regulation.
Another point – many at least with pots report a worsening of symptoms during a weather change or a cold front build up to a storm. This is commonly reported in rheumatoid arthritis and ankylosing spondylitis where cytokine-driven destruction of joints and connective tissue is at play?
what if pots/cfs/fibro is a cytokine driven inflammatory attack on regional small fibers in some cases? Waxing and waning, etc.
the whole sfn concept has been bombarding the pots boards for a while – that and fatigue from reperfusion injury post orthostatic intolerance.
And finally I was skeptical of sfn in my case until a neurologist touched a cold piece of metal on my outer upper leg, shin and then bottom of foot where I could not distinguish temperature in any way.
All of the symptoms and conditions listed above are very real, and they likely have different root causes for different people. Now that I’ve given that disclaimer, everyone with fibromyalgia, CFS, POTS, any sort of autoimmune disease, lymphoma, anxiety, etc. should look through their medical records to see if they have ever taken a fluoroquinolone antibiotic – Cipro, Levaquin, Avelox, Floxin and a few other less commonly used ones. Here is why:
In August, 2013 the FDA updated the warning label on all fluoroquinolones to include warning of PERMANENT peripheral neuropathy. This includes small fiber neuropathy. http://www.fda.gov/Drugs/DrugSafety/ucm365050.htm As you noted, POTs and autonomic nervous system dysfunction is related to peripheral neuropathy.
The root of the damage from fluoroquinolones is damage to mitochondria. This article, http://www.jimmunol.org/content/184/9/4827.full.pdf, notes that, “ciprofloxacin was also shown to deplete the mitochondrial DNA (mtDNA) content, thus leading to mitochondrial dysfunction and retarded cellular growth (15–17).” Mitochondrial dysfunction can lead to chronic fatigue, as mitochondria are the energy centers of cells.
Per the same article, “Ciprofloxacin treatment was shown to exert various effects on activation- induced gene expression in T cells (10). Stimulatory effects of immediate ciprofloxacin treatment (incubation time up to 72 h) on basal expression of IL-2, TNF-a, or IFN-g in mitogen-activated T cells have been reported (11, 12, 24).” This means that immune system cells are stimulated and an autoimmune disease is brought on by these drugs. Here is an additional article on the topic – http://aac.asm.org/content/42/8/1923.full
Mitochondrial damage can also lead to a variety of other health problems. Please see this article – http://psychrights.org/Research/Digest/NLPs/DrugsCauseMitochondrialDamage.pdf
Please feel free to contact me if you have any questions. More information can be found on my blog, http://www.floxiehope.com.
Thanks!
Until I was fully seeing patients with neuropathy and dealing with the families and support structure which exists in families, I fully didn’t understand the extent that neuropathy affects families. All of the different types of neuropathy, but especially diabetic neuropathy has been really life altering.
I appreciate this type of article which really outlines in scientific and thought provoking ways, the causes and possible treatments which can help patients who suffer with neuropathies of all types. Thanks again.
I have recently become involved with, in addition to nutritional therapies, an FDA approved device called Calmare. Has anyone heard of it? What are your experiences? My info comes from http://www.saltlakechronicpain.com
I look forward to your replies. Thank you.
Thanks Dr. Page,
I look forward to checking out Calmare. Two more studies recently came out on SFN in FM. That will covered in a blog probably tomorrow.