

The ME/CFS Association in the Netherlands brings its De Meirleir video series to an end with its 20th video on Testing in ME/CFS. After Dr. De Meirleir their ME/CFS Experts video series is moving on to Dr. Visser, a cardiologist (see below). Congratulations on a well-done series!
- Find the text of the entire De Meirleir series here.
Dr. De Meirleir on Tests You Might (or Might Not) Want to Get Done
The ATP Levels Test
“It’s practical use to me seems limited”
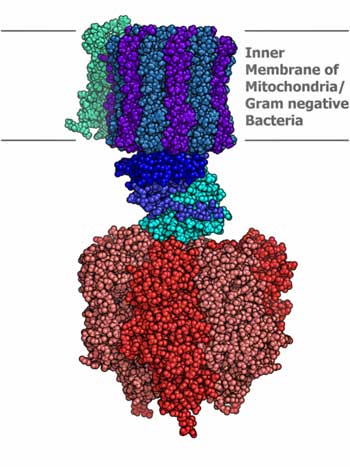
Energy production and the mitochondria is a pretty hot topic in ME/CFS, with several supplements intended to increase ATP production in common use. Decreased CoQ10 levels have been found in both chronic fatigue syndrome and fibromyalgia, and Dr. Teitelbaum touts D-Ribose , a mitochondrial enhancer, for ME/CFS/FM.
The question is, though, should you get your ATP levels checked?
Citing the high variability of ATP production in cells, Dr. De Meirleir suggested you should not, unless the test was being used with an intervention designed to increase ATP levels. Citing the low ATP levels that are found in many chronic illnesses, though, it was clear De Meirleir doesn’t believe reduced ATP production, while it may be present, is the problem in ME/CFS.
If low ATP levels are found, they could provide the basis for symptomatic treatment that provides relief. You may not be curing ME/CFS by increasing ATP production, Dr. De Meirleir said, but it could help you feel better.
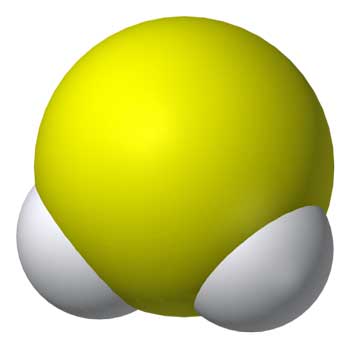
Hydrogen Sulfide
Dr. De Meirleir created the hydrogen sulfide test for chronic fatigue syndrome, and for a time it was being talked about as a diagnostic biomarker. The test picks up metabolites of hydrogen sulfide gas in the urine and provides an assessment of Th1/Th2 functioning. Eighty-five percent of ME/CFS patients test positive for Th2 dominance on the H2S test.
The gut, of course, is often called the ‘second brain’ because it’s loaded with neurons. Could a similar level of neuronal ‘excitation’ in the gut be producing H2S? Dr. De Meirleir did not say why H2S levels were high in ME/CFS gut but it’s probably not doing anything good; high H2S levels in the gut have been tied to both colitis and colon cancer..
Dr. De Meirleir did not talk about one of the issues proposed by the originator of the H2S theory in ME/CFS, Marian Lemle; central nervous system dysfunction and fatigue.
Marian Lemle’s interest in H2S started when she learned of its ability to send animals (and humans) into a torpor-like state similar to the fatigue found in ME/CFS. This torpor-like state is induced, it’s believed, to protect the body against overly high metabolic demands and oxidative stress.
It turns out that central nervous system excitation causes neurons to pump out H2s as a protective measure. A similar process happens in blood vessels faced with high rates of oxidative stress. The low blood volume in ME/CFS could create ischemic conditions that produce high rates of oxidative stress, and indeed, studies do find increased levels of oxidative stress in ME/CFS.
A similar process occurs in sickness behavior when the brain induces fatigue and flu-like symptoms to cause the body to rest and not spread an infection. The process in sickness behavior is believed to be driven by cytokines, but cytokine results in ME/CFS have been quite variable. (A recent study found no evidence of cytokine upregulation after exercise or poor sleep in ME/CFS.) Could the torpor in ME/CFS be driven by H2S overproduction?
What about the mysterious ‘chronotropic incompetence’ sometimes seen in ME/CFS? Chronotropic incompetence refers to the strange inability of some ME/CFS patients to get their heart rates up to speed as they exercise. While this is typically seen in heart failure, the heart is clearly not the problem in ME/CFS (see below). Lab studies suggest hydrogen sulfide can have just this effect.
This is all highly speculative, but Suzanne Vernon and other researchers received Marian Lemle’s theory with real interest. H2S – in both the gut and the brain – is another possibility in ME/CFS.
Natural Killer Cells
Not only does natural killer cell dysfunction run rampant in ME/CFS, but NK functionality can, in some patients, be shockingly low. Natural killer cell dysfunction is not the complete answer to the immune problems in ME/CFS – some patients can get their NK cell functioning up without seeing much improvement – but having our earliest responders to viruses and cancers not working well is a significant problem.
De Meirleir noted, again, though, that while NK cell dysfunction is important, it’s not – citing chronic Lyme disease patients with similarly low levels of poor NK cell functioning- specific to ME/CFS.
NADH
“The research team proposed using serum NAD(P)H to monitor metabolism and fatigue status in patients with CFS. Following patients’ NAD(P)H levels over time may aid in selecting therapeutic strategies and monitoring treatment outcomes.” Mikirova et. al. 2012
De Meirleir noted that the NADH test (NAD/NADH ratio) could indicate that early acidification of the muscles was taking place during exercise, and could explain, interestingly, the alcohol intolerance in ME/CFS – which De Meirleir asserted is present in nearly 100% of ME/CFS patients.
Low NADH levels were correlated with low COQ10 levels in a recent study, suggesting NADH test results could be an analogue for COq10 levels (and that both these supplements could be helpful).
NADN supplementation, however, significantly improved only anxiety in ME/CFS in a recent placebo-controlled trial. An earlier trial found dramatic improvements in the first trimester, but no difference between controls and those getting NADH after that.
Dr Visser – Dutch Cardiologist Pt: I – Chest Pain and Shortness of Breath
Dr. F. C. Visser had been a Dutch cardiologist for over thirty years. About five years ago, he switched full-time to the research and support of people with chronic fatigue syndrome (ME/CFS) or, as he calls them, ME patients.
The ME/CFS Association will feature Dr. Visser in five more video’s on cardiac aspects of ME/CFS. Dr. Visser’s current study featuring two-day test-retest exercise studies, makes him one of four researchers/research groups (Workwell, Vermoulen, Visser and Keller) that I know of that are exploring this potentially game-changing area.
Chest Pain
“A Cerebral Phenomenon”
Dr. Visser may be – probably is – the only cardiologist in the world with such an intense focus on ME/CFS. Calling the high degree of chest pain found ‘extraordinary’ in the younger population he treats, Visser noted an earlier English study found it was present in 80% of people with chronic fatigue syndrome.
The pain usually occurs on the left side of the chest, close to the cartilage on the sternum near the second and third ribs. He finds it in 40-50% of his patients.
Asking what’s causing this problem, our ME/CFS cardiologist laid out three possibilities: an irritation of a small joint between the sternum and ribs, lymph node drainage problems, or a complication of orthostatic intolerance.
“None of the above,” our good cardiologist asserted! That pain in your chest (which I experienced for years) is simply an aberrant pain signal generated from the brain – a cerebral phenomenon. How he figured that out, unfortunately, he didn’t say.
Before telling us how to treat chest pain in ME/CFS Dr. Visser noted that he’s seen some 2,000 ME/CFS patients, and in all those patients he’s never seen severe heart problems such as obstruction of the arteries/veins, pericarditis, or lung problems. You may have pain associated with the heart area – and if its severe get it checked out – but ME/CFS itself is not a disorder of the heart.
For myself I ended up once at the emergency room and once at a doctor’s office with what I thought were heart-associated pains, but nothing was found.
What to do about this mysterious brain-caused pain? Nothing! Unless it’s really severe – then use pain killers.
Shortness of Breath
“It is purely a wrong signal.” Frans Visser
Shortness of breath is another common finding in ME/CFS. I no longer experience shortness of breath, but I remember vividly very short and rapid breathing patterns that would come on. It was as if some little engine had taken over my lungs and there was no slowing it down. It didn’t happen that often and eventually it completely went away.
Visser stated shortness of breath occurs in about 50% of ME/CFS patients
Calling shortness of breath a complex interaction between the heart, lungs, circulation, and yes, the brain, Visser stated that something, somewhere – no one knows where – had gone wrong in that interaction, sending the breathing pattern off.
But, given that defects in the heart and lungs are rarely seen in ME/CFS, you can scratch those two major organs off the list (thankfully). This is a problem mostly caused, apparently, by an interaction between the brain and the circulation. In short, Visser stated, it’s a signaling problem generated by the brain. The heart and lungs are fine.
Again, Visser did not suggest any treatment.
Conclusions
Our ME/CFS cardiologist has labeled two seemingly heart/lung associated symptoms not as heart issues but as ‘signaling’ problems, both associated with glitches in the brain and the nervous system. It’s an interesting beginning to what will surely be an interesting video series.








But what about real CVS problems, I thought it was one of the three most common causes of death in people with CFS?
I don’t know…I think the cardiovascular system is key – but it may not be the heart or the lungs. Workwell doesn’t find evidence of heart and lung problems either; maybe – it’s all signaling….????
Well, I’ve developed a Dialated Cardiomyopathy and It’s my understanding that it’s one of the three main causes of death in CFS. I don’t think that’s signaling.
I think dialted cardiomyopathy by CFS is due to chronic uncontrolled tachycardia. CFS patiënts i know have a little thickness and stifness of the left ventrikel. Also due to tachycardy.
I too thought the same thing, cardiac arrest just might be the first cause of death among ME patients, and at times I feel I could well trigger one just by running up the stairs.
A wrong signal from my brain? I prefer not to try and see.… Dr Visser seems to be saying in his own way that it is “in the head”, physiologically speaking of course. As a cardiologist he saw tons of patients with real heart conditions in his career, such that he could underestimate the reality of the problem in the case of “chronic fatigue”.
The aberrant chest pain for us, originates in the stomach. Stomach soothing herbs, such as Slippery Elm and Marshmallow Root, plus Ginger, on an empty stomach, can be a very significant help, even in the middle of the night, to get back to sleep. I add a little food at that time also, such as piece of cheese or warm milk. It’s safe and it works.
The cardiologists always ignore the autonomic nervous system located in the gut, at our peril.
Remember, the autonomic nervous system also controls the diaphragm, that we breath with!! It depends a lot on minerals and fatty acids and hydration. Avoid sugar and gluten. RP
Thanks Rich…would those things work for problems lower down – irritable bowel?
For what it’s worth, I think the ANS is key as well.
My gluten avoidance has gone pretty well; less but gut problems but then something went kablooey last night – I had bloating like I couldn’t believe…I thought I was going to burst 🙂
I think it would help with the IBS. Soothing the gut seems to help all around.
No doubt, something you ingested caused an inflammatory response. It happens to me when I forget to read the label. Modified food starch can be wheat, for example.
The older we get, the more compromised all systems become.
A food reaction test is paramount, in my experience.
My fogy brain can’t recall the best one at the moment. When it comes to me, I’ll let you know.
RP
My IBS has definitely gotten much worse over the years. Thanks for the Alcat test…
Google the ALCAT test! RP
Thank you Rich, that seems like good advice and makes sense. The breathlessness and chestpain with me usually start after even some little exercise. My heart and vascular system was totally checked out and there was no problem found. Last time I visited my doctor about these symptoms she seemed to think that it could be due to a hernia or sinusitus. She also seems to think that it is all due to lack of exercise eventhough I exercise as much as I possibly can and am not even pacing myself, just going through my day as good as I can, my diagnosis is fibromyalgia. Anyway thank you for this insight about soothing foods, I will certainly try. What you say makes a lot of sense to me.
This is such good info for me right now. Last October I suddenly had chest pain and SOB for 5 days. Was convinced to go to Urgent Care. That doc misread my EKG and sent me to the ER in an ambulance, thinking I was having a heart attack. ER doc said EKG wasn’t normal but wasn’t concerning. They did do a lung scan checking for an emboli and instead found a very rare congenital growth on my lung that was very infected, called a Sequestration, that I had to get out a few months later. But all this time the chest pain continued so finally followed up with a cardiologist. Nuclear stress tests and stress echo all totally fine. They said the next step would be an angiogram but I was convinced ( more than ever now) they wouldn’t find anything so never had it. I’m 60 and have had CFIDS for decades and never an issue with this, and am so glad to know it’s most likely just part of the CFIDS. Have also been wondering what tests my PCP could order for me that might dig deeper, without having to go to a specialist, so will check out Dr. Meirleir’s series. Thanks Cort.
Betsy Keller, Ithaca, NY?
Yep…that’s it – I’m amazed I couldn’t remember her name. Thanks
No, I’m from Colorado Springs, CO.
I think we must have a couple of Betsy Keller’s 🙂
Hi Cort, I should have said I’m Betsy Kemp from Colorado Springs. So there’s probably just one Betsy Keller. 🙂 I see you’re up in Broomfield now – maybe we’ll meet one day. There was recently a talk in Denver the CFIDS Association gave.
Visser’s “no CVS” verdict seems to be focused on classic heart attack situations. Certainly heart infections in me/cfs have been documented, and at least one death in a young adult has been well-documented in the US. Perhaps heart infections are outside Visser’s interests.
Also, I seem to recall that some characteristic of the disease tends to affect endothelial tissues adversely, which could in turn contribute to stroke or plaque-provoked events (which gets us back to the classic heart attack.) Unfortunately I cannot remember the characteristic at work.
I greatly appreciate Visser’s words on the chest pains perhaps caused by events in the brain. It is good to have something not to worry about.
The following has nothing special to do with me/cfs, but on the subject of heart attacks please keep in mind that gall bladder attacks produce very nasty chest pains, and many doctors are surprisingly unable to call to mind gall bladder as a possible diagnosis. An ER resident gave me Tagamet for my first-ever attack, which was like giving someone Neosporin for tonsilitis.
Good points Deborah…I do recall Lassner’s interesting work out of Germany suggesting viral attack of the heart was something that should be investigated in ME/CFS.
The rest of Visser’s series is going to be interesting – 5 more web seminars focusing on different symptoms and orthostatic intolerance, I believe.
I watched all the video presentations of Dr. Martin Lerner who also suffered from CFS. He had a biopsy done of his heart (and had complications from it) which he claims was virally infected – I don’t remember which virus, maybe it was EBV. Also, Dr. Klimas told me that most CFS/ME sufferers were a unit low in blood volume which I assume would cause shortness of breath or even orthostatic intolerance. I wish there were more biopsies, in fact it seems to me some autopsy work on patients who die that have CFS/ME could be very illuminating as to the possibility of nerve or organ infections with a number of viruses.
Agreed Kathe….I imagine that would be happening if ME/CFS was an illness that got full interest from the medical world; I think they would be doing autopsies right and left to try and track down what was going on.
That’s right about Dr. Lerner – once again, we have different opinions and experiences from two experienced doctors….
When I was sent to the ER they had to admit me to get the lung scan because I’m allergic to IVP dye. They tried doing a stress echo the next day but aborted it and put me on the cardiac ward for 2 days because I had to go to the bathroom after the echo and before the treadmill and when I got back my heart rate had gone up about 30 or so beats per minute. I didn’t think anything of it at the time but am wondering if this could be CFIDS related too. I have no subjective symptoms or would ask for a tilt table test. Maybe Visser’s series will shine some light for all of us.
The problem is that when you don’t distinguish between ME and CFS, if 50% of the group has some complaint this probably has nothing to do with ME.
Chest pains and shortness of breath are not characteristics of ME. Orthostatic intolerance is.
But how is the viewer going to make the distinction?
Yes I think there is a heart problem. Dr. Cheney is finding the 97% of his patients have diastolic heart dysfunction and venous insufficiency. So wouldn’t that sound like we have a heart problem?
Those of us with POTS (postural orthostatic tachycardia syndrome) for sure have chest pains, orthostatic issues, tachycardia etc.) They tell us our hearts are fine —except they beat so fast with upright posture that you wonder how many beats we get in a lifetime and are we using them up way too fast????? Some of us have mitral valve issues.
The other thing that some of us with Mast Cell Activation Syndrome (MCAS) have is Kounis Syndrome. It’s where the mast cells somewhat attack the heart. It’s really considered rare. But, I had this happen and spent the night in the cardio unit. They thought I was having a heart attack as 2 under the tongue nitroglycerin doses and a patch for 16 hours calmed down my high blood pressure and heart rate. I also had an IV and LOTS of antihistamines. There was no heart muscle damage and it was not a heart attack. Guess what the treatment for Kounis Syndrome is.. . . . nitro, antihistamines and IV’s. (Difficult treatment for a POTS person. But, was very necessary.) I now have epi pens and use daily H1, H2’s and GastroCrom and lots of supplements that help with histamines. Also, change of diet.
http://www.medscape.com/viewarticle/732843
http://en.wikipedia.org/wiki/Kounis_syndrome
http://www.ncbi.nlm.nih.gov/pubmed/22050066
Those of us with POTS also have issues with our breathing and shortness of breath.
Issie