



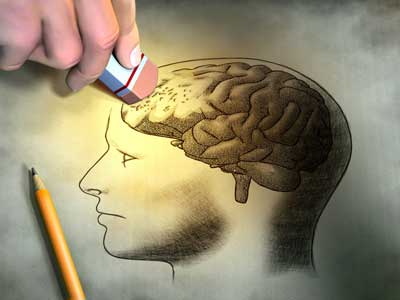
In Part II of the A Neuropsychologist Looks at ME/CFS, Dr. Lange looks at neuropsychological testing, IQ, we riff on how cognitive problems can affect how well you move, and more…See Pt. I below.
Neuropsychological Testing

The Three Major Cognitive Hits in Chronic Fatigue Syndrome
- Inefficient information processing
- Low working memory
- Reduced executive planning
Oddly enough, memory issues, which at first blush seem to be big, are not; people with ME/CFS do have the ability to remember things they’ve retained – it’s the retaining part that’s the problem.
The cognitive problems in ME/CFS mostly involve processing information – how quickly you can do it and how much you can process at a time. If you can’t process information as quickly as before, and you have a smaller working memory as well, you’re not going to be able to take in as much in as before. Basically you’re slower, and you can only handle smaller bits of information. Whereas before you could hold a paragraph in your working memory, now it may be down a sentence or two. It’s not that you don’t remember it – you never got it in in order to remember it.
IQ Intact!
It’s interesting that IQ is hardly affected in ME/CFS – you can still, given enough time, figure out problems. The problem, again, is retaining the problem in your mind long enough to be able to figure it out. Dr. Vernon noted that when she was at CDC they had trouble finding tests for the patients to fail because the patients were ‘too smart’. Dr. Lange concurred that many of her patients are above average intellectually.
At this point let’s note that no one to my knowledge has asked an ME/CFS patient to do the cognitive equivalent of a two-day repeat exercise: i.e., no one has tried to simulate a ‘working environment where mental endurance comes into play. The CDC multisite study is going to challenge ME/CFS patients with an exercise test and then measure their cognitive capabilities.
Riffing on the ‘Brain/Body’ Component in ME/CFS
Most studies (but not all) suggest that the cognitive abnormalities present in ME/CFS are relatively mild, but those tests may be missing something.
Dr. Lange noted that these deficits could affect motor functioning or movement, as well, and some studies suggest that ‘motor planning’ could be affected in CFS. Movements do not just happen – before you make a movement it’s been planned out in your brain. But what if motor planning is impaired?
The Executive Functioning/Motor Planning Connection
A cognitive process called executive functioning involved in ‘planning’ has taken a hit in ME/CFS. Executive functioning includes the ‘automatic’ functions you usually don’t think about such as driving a car, cooking a meal, putting the dishes away, using an ATM machine… and walking.
A fascinating series of recent Alzheimer’s studies suggests cognitive problems may be translating to issues with movement as well. Researchers are now thinking that slower than normal walkers may have a hidden cognitive problem, and that most cognitive tests are missing an important component: the body.
“People who are focused on cognition largely never watch people move. The tests are all done sitting down. But damage to the wiring is an important shared problem of difficulty with thinking and difficulty with moving.” Dr. Studenski
A 72 year-old woman passed a walking test with flying colors but when she was asked to count backwards while walking, her rhythmic gait collapsed. Dr. Stephanie Bridenbaugh, head of the Basel Mobility Center, said,
“She teetered and wobbled on one foot. She almost tipped to the side and she didn’t notice any of it. She was mad that she didn’t remember more numbers.”
These findings reinforce the need for patients to be tested in complex environments. People with ME/CFS may do relatively well in simple tests, but asking them to count backward from 50 while walking might get very interesting.
Dr. Lange stated that, as far as other conditions go, the deficits found in ME/CFS are relatively subtle, but they show up more when we’re doing complex tasks (including perhaps walking and talking), and, in fact, researchers are now using more and more complex tests.
The Cognition and ME/CFS Webinar
Western Researchers Missing A Key Test?
Remember the dozens of different neuropsychologists tests Dr. Vernon referred to part I of this blog. A Japanese study that found not subtle but major cognitive deficits in chronic (cognitive) fatigue syndrome suggests researchers may be missing an important test. The study – which employed a ‘dual’ test (‘Kana Pick-out Test’) which requires far more cognitive resources than a single test – found startling cognitive deficits with the worst patients exhibiting dementia and even the best scoring patients scoring far below the mean. A dual test – by taxing different parts of the brain at the same time – exposes brains which have lower levels of resources.
- Dig Deeper: Japanese Sensory Gating Study Reveals Profound Cognitive Deficits Present in Chronic Fatigue Syndrome
One wonders what kinds of environments might throw movement off in ME/CFS. High stimuli environments? How about being upset or anxious or thinking furiously? How much do these distractions affect our energy levels and ease of movement?
The Medication Cognition Hit
Are Western neuropsychologists missing a key test that would reveal high levels of cognitive dysfunction in ME/CFS?
Many very sick patients are on numerous pain and other medications some of which can affect cognition. Dr. Vernon noted that nobody has a clue what kinds of interactions can occur between multiple drugs. Dr. Vernon has been around the medical field for quite a while, but even she was startled by how many drugs some patients were on.
Dr. Lange suggested that patients ‘ask, ask, ask’ about the potential side effects of meds. In his Ottawa talk Dr. Clauw said one of the first things he does with patients is get them off any unnecessary medications, and the guide he uses is ‘functionality’. If being on the drug has made you more functional then fine; if it hasn’t then you might consider getting off of it.
Finding the Right Neuropsychologist
The deficits in ME/CFS are rather peculiar, and because of that, standard neuropsychological testing – a foundation of disability testing – needs to be done correctly or you could blow your case. Most neuropsychologists are not up to speed on the cognitive deficits in ME/CFS. Dr. Gudrun Lange knows the right tests to use, and Dr. Cheney has used Taras Onischencko’s services in the past. If you know of an ME/CFS-knowledgeable neuropsychologist, please let us know in the comments section and we’ll build a page on them.
Good neuropsychological testing is usually quite time-consuming and expensive. Dr. Lange does a full 8-hour battery in new patients, and then a second 2-hour round of testing that focuses on ME/CFS-specific problems (i.e., processing speed, working memory, information processing). She always includes something called a Validity Indicator Profile (VIP) to establish that patients have put forth the requisite effort and to dispose of any ideas of malingering.
Evolving Brain Technology
The brain is the most complex organ in the body, and researchers have a long way to go to be able to understand it, but they are making progress. The emphasis now is to attempt to the capture the brain as it is – not as a collection of single circuits but as a highly networked organ. Imaging studies are underway, one of them in CFS, that attempt to capture the brain holistically as a collection of interconnected neural networks. The big brain initiative sponsored by the federal government will be more focused on interconnections in the brain than in the structure of the brain.
Increasing One’s Cognitive Abilities
Is it possible to increase one’s cognitive capabilities? Studies suggest that different exercises can help people with chronic illnesses reduce their brain fog and help them to think more clearly and efficiently. Much more extensive studies need to be done, but Qigong, for instance, helped improve self-reported ‘mental functioning’ in fibromyalgia.
Brain games
Some studies have shown that brain games do help. Lumosity helped executive and memory skills in children with cancer, but overall the evidence is limited.
Clinical Trials
Alzheimer’s is pushing the envelope on efforts to regain one’s cognitive capabilities. From experimental drugs (MSDC-0160 – a brain glucose enhancer) to acetylcholinerase inhibitors (Donepezil, mifepristone), to nicotine receptor agonists (varenicline), to repetitive transcranial magnetic stimulation (rTMS) to nasal insulin to supplements such as resveratrol and omega three derivatives, researchers are throwing as many drugs, machines, and supplements as they can at people in the early stages of Alzheimer’s, hoping they can improve their mental functioning. This field will bear watching.
The Stress of Poor Cognition
Being unable to think as clearly as you used to can be stressful. Our working memory allows us to store enough information to stay focused and understand and complete our tasks; i.e., it allows us to ‘get into the groove’ during a task and get it done. Not being able to get ‘into the groove’ is obviously inherently frustrating.
One researcher, Elbert, noted that “If your working memory is reduced, you’ll have difficulty having a cool response—in thinking it completely through—because you don’t understand what is really going on. You’ll respond more with an angry outburst to a stressful situation. This is how humans adapt to a threatening and adverse environment.”
Those upsets, frustrations and fears that come with reduced cognition, simply take up more of the limited mental space that is available. Being able to deal with them more effectively might very well free some mental energy not just for the tasks at hand but also for things as simple as walking, moving, etc. That leads us to ways of dealing with these inevitable upsets.
Mindfulness Meditation Exercises to Improve Executive Functioning
By clearing the mind of distractions, mindfulness meditation exercises could conceivably allow scarce resources to flow to and assist with executive functioning, and possibly even increase ease of movement. Could exercise that combines meditation and movement like yoga,Tai Chi, or Qigong give movement a boost?
Some studies suggest these practices can provide some help. Meditation or mindfulness training can improve executive functioning, one of the key cognitive processes that’s gone awry in ME/CFS/FM. Mindfulness training can increase one’s working memory (ability to retain information) and improve ones ‘focused attention’. Given study evidence that brains of people with FM/ME/CFS have difficulty switching off their attention to innocuous stimuli – thus limiting their ability to fully concentrate on the task at hand – finding a way to increase ones ‘focused attention’ would be a good thing.
http://www.youtube.com/watch?v=ErcJCI-sm_A








Has anyone tried the Gupta retraining program and if so did you see any improvement? Thanks.
Yes, I’ve been doing Gupta for about 6 weeks. It has definitely helped me become less negative and has seemed to lessen my anxiety, both of which contribute to the condition. The program combined with strict pacing has made me feel maybe 15% better so far. Not to mention, my sleep has improved which also helps. I started it after a terrible crash in which i was so negative and I could see it was that negativity that was making my symptoms worse. I figured what do I have to lose as it is a money back guarantee. I believe in his hypothesis as when a crash comes on I feel the adrenaline rush….I recently went to one of the major research hospitals and my doctor believes that CFS all stems in the brain. He said my brain is now different than his. So, this reinforced to me that Gupta is really on to something and I hopefully can use his program to make new neural pathways. We’ll see…Gupta says give it 6 months with the goal of becoming less negative, not the goal of becoming healed.
My brain is certainly different than it used to be – there’s no doubt about that:).. My belief or rather my experience is that our systems are so sensitized that it’s very easy to throw them into turmoil causing all sorts of symptoms. My guess, at least for myself, a kind of stress-sensory disorder aspect is present.
Good luck with Gupta; all these kind of mindfulness practices take practice, practice, practice and time:)
Thanks Lesley and Cort – maybe I’ll give it a try. I could use a dose of positivity but won’t expect a cure.
I’m seriously thinking of doing the Gupta training, as well. Watched the free intro videos this week…I get so very negative, but I didn’t see any cases in the testimonials of people that had been ill as long as I have…Makes me wonder if I’m “too far gone” to get better, but I’m desperate, so what the heck~it can’t hurt.
If stressfull patterns of thought are present they can be changed in anyone..I use a variety of techniques from Buddhism and Landmark Education to get at them.
However it turns with regards to your healthy and actually I fail to see how reducing stress could not be not helpful (at least in my case) – there’s just the sheer quality of life aspect. Why not have as high a quality of life as possible?
Good luck with whatever you decide to do.
I tried the program. I was at my wits end, my nervous system was totally freaked out. I’d watched the intro videos, felt like this was my best chance. I’ve also had many years of many therapies pre- ME/CFS. Initially the Gupta sessions made me even more anxious and agitated. I found it aggravating. Shortly thereafter I discovered GAPS diet. 3 days after stating the diet, which also freaked me out, my nervous system calmed. I then did the Gupta program for a short while. Because of my past experiences with hypnosis and similar things, I was hyper-sensitive to some of the wording, and had to force myself to relax and accept it. However, all my real gains were from my shifting biochemistry. My next big gains were when I supplemented for pyroluria and later B12 protocol. Each of these things reduced my anxiety and negative thoughts. It turns out all my issues have been biochemical. It was most certainly not my mind that was preventing me from worldly pursuits. I’ve not returned to Gupta, don’t know if I will. Best to you, ahmo
Congratulations for finding something that helped. Thanks for passing it on 🙂
“Executive functioning includes the ‘automatic’ functions you usually don’t think about such as driving a car, cooking a meal, putting the dishes away, using an ATM machine… and walking.”
That just reminded me of my Psych undergrad days when we were covering the neuropsychology of movement. Particularly how we become ‘expert’ at physical tasks to the extent that they become automatic. You never forget how to ride a bike do you? Or do you?
Remember back to learning to drive particularly changing gear with a manual gearshift. At the start you almost have to verbalise the stages – decelerate, depress clutch, engage gear etc etc. In time these stages become ‘chunked’ into what are called motor programs – discrete modules of body memory that can be deployed automatically with all that’s required additionally is a little fine tuning depending on local circumstances (reaching and picking up a cup is the same motor program but with a little fine tuning depending on the size, weight, full or empty etc).
I wonder if retrieving these ‘motor programs’ is affected or maybe we need to attend to the fine tuning more than is normal. When I’m about to crash my walking follows a predictable pattern. I I get episodic ataxia. I slow down and develop a limp in my right leg (never injured). Then I slow further to almost a complete stop and all of a sudden I have to concentrate on each individual element of balance and walking. Its as if I need to attend to each miniscule detail of staying upright and moving and uneven ground feels like a minefield.
Never mind riding a bike – how do you forget how to walk?
This is in parallel with an almost complete mental shut down. I’m not in any way deconditioned so I can pretty much rule out muscle fatigue even though my legs will feel like lead and my muscles will ache.
All pretty subtle stuff really 8 )
Cort, I had a neurocognitive exam when I first got to the point that I couldn’t put two and two together, shortly after I quit working as an RN, which I did because I knew I was going to make a mistake. My own mother insisted I have it done when it was recommended by my psychologist because she was certain I had Alzheimer’s. Now mind you, this was done before I had a definitive diagnosis of FM or CFS, and I wasn’t on any medications other than those to treat migraine and an occasional pain pill. The test was administered by a forensic neuropsychologist, the Cadillac of all neuropsychologists.
The findings were that ranked at the lowest level of short term memory retention and a bunch of other things that I can’t remember right now. The report was like 20 pages and the test was a grueling 8 hours. The good news was that my IQ was intact and I didn’t have organic brain disease. The bad news was that it was recommended that I would be a danger to others to practice as an RN, (and at my age and my cognitive deficit, I was not trainable.) This is why I started writing, to maintain what I had left, but the truth is, it really hasn’t made a difference. I am big into meditation and mindfulness, but that hasn’t made an iota of difference either. I literally have to set a timer if I put something on to cook, because I just do not remember. My husband follows me around like a hawk and is afraid to leave me alone. I am afraid to be alone. I cannot navigate anymore and I used to be a fantastic co-pilot. I cannot tell you the number of times I have gotten lost going to familiar places. I literally depend on spell check and grammar with MS word and don’t go anywhere, even to my aunt’s house without using a GPS. It is disparaging, but I hold on knowing I do still have my IQ and some don’t.
The test did validate that what I experience is real. If for nothing else, it was worth that.
In healing and hope to all, Celeste
As a former Mensa member and nurse practitioner, I’m often found wanting in all the areas you mention above and the contrast is extremely frustrating, to say the least. I had to leave a profession I loved long before my time because I could no longer trust my memory to recall, or my speech to explain, the details of medical treatment to a patient.
However, mindfulness meditation training keeps me from self-recrimination, even frustration most of the time. I can keep simple paragraphs in my mind, like novels, and only occasionally lose the ability to comprehend research papers (although I read much slower now and cannot recall the particulars 15 minutes later), so the memory aspect appears to be validated in the this sample of one.
Cognition aside, meditation training and practice allows me to traverse the difficult pathway of this disease with more peace and acceptance than I could have before I started sitting. I highly recommend it.
A FORMER Mensa member – ha! – Glad to hear meditation/mindfulness practice has helped…Peace and acceptances is a good thing – a precious thing if you can achieve it. I’m working on it 🙂
Marco, the same thing happens with me and ataxia. If I’ve overdone it, am tired, or having a POTsie day – it’s like my legs freeze up. Almost like my feet glue to the floor and walking is a very “mindful” thing that I have to concentrate on to accomplish. I literally drag my legs and am worse on the right side too. Wish I knew what that was all about. I do have a meningioma on my left frontal lobe and I know the left side of the brain affects the right side of the body —but, I don’t think that really has anything to do with this. As if that were it, it would happen all the time. It happens mostly when under stress or being overly tired. Also when I’ve overwalked. It’s like my muscle strength just gives up. I can consciously say to myself – pick up your foot, swing your leg and sometimes it just doesn’t work. (This hasn’t happened in awhile for me. Thankfully.)
As for the testing of brain comprehension. My sisters kids who also have forms of dysautonomia —have ADHD and one of the boys was found to have dyslexia. Did you know there are at least 3 kinds of dyslexia? There is hearing, seeing and one other one that I can’t remember (LOL – brain fog today – figures with me trying to talk about memory).
http://www.macalester.edu/academics/psychology/whathap/ubnrp/dyslexia/types.html
My father also has this and as he ages it has gotten worse. The docs say it’s his comprehension that is messed up. He hears you talking – but, that sounds like wha wha wha wha to him. It makes no sense and you might as well not be talking to him. It’s like he will sort of stare through you when this happens. There are some people with POTS that are being found to have absent seizures. This is the how a person is when one of those happen. There must be some sort of connection and how is it that families “inherit” it? With myself, I notice that sometimes I will type the wrong letters and it’s always the same misspelling of things I’ll use a b instead of an m —like for the word my. Sometimes, I miss it with rereading too. It will look okay to me.
Issie
I have long experienced a kind of freeze-up or lock up feeling in my muscles. I don’t know if it has to to do with fear or what but it’s what made Marco’s piece of the Stiff Person Syndrome resonate with me. It is associated with stress with me but I think small bits of it are present alot and it impairs graceful movement for me – and I think it greatly increases the energy need for movement.
have you ever tried to dance when that happens? Spike Milligan [a UK famous comedian] who had Parkinson’s said that he could still dance when he got to that ‘can’t walk’ extreme. Something about walking and dancing using different memory pathways.
No, haven’t tried dancing. But, my first WRONG DX was Parkinson’s and then the next WRONG DX was Multiple System Atrophy. And after 3 weeks at Mayo the first time and then 2 more week long visits and thousands of dollars – got the POTS DX along with EDS and MCAS. That one fits better than anything else. With autonomic nervous system malfunction that affects your whole body —that can explain a whole lot.
When my hubby is with me, he actually takes me by the hand and arm and supports me. Sort of pulls me along. Usually I have tremors at the same time when this happens. When this happens, I have to physically pick my legs up with my arms to get into a car. Sit down first and then manually move my legs. If I’m by myself – I just have to sit and wait for things to get better. Try to get to some place to sit and a quiet place to settle out. I usually know when it is going to be a bad day and just stay home.
Issie
I’m working my way through a complex but very interesting paper on complex regional pain syndrome at the moment – something you mentioned in comments to one of the previous articles.
The authors propose autoimmune mediated ‘spreading neuroinflammation’ as underlying the various symptoms of CRPS. Thinking about the tremors and how we both seem to suffer from some sort of ‘transient ataxia’ (‘normally’ I have few problems walking) these excerpts might be relevant :
“The movement disorders associated with CRPS include fixed dystonia, myoclonus, and tremors.”
“Microvascular lesions in the brain and spinal cord may be a common way for individuals with neuroautoimmune disorders to have transient neurological and neuropsychiatric events, including movement disorders”
I know I have autoimmune disorders and working on that aspect of my illnesses has helped me more than anything else I’ve tried. When I get in a flare – all the known autoimmune things start to get worse for me.
I really do think autoimmune issues and inflammation are part of the two key elements in all of this.
Looking forward to reading what you come up with on CRPS. I didn’t realize that was connected with tremors. As for pain, I have LOTS of it – but, I always just write it off as EDS and FMS. But, it would make sense if CRPS is associated with autoimmune this could be a likely thing as to reasons.
Issie
i want to get in on this thread, but i need more time
Yes! to so much of this. If normal people only knew that !/we can forget how to drive a car, how to organize packages or objects to carry them, how to handle a fork and knife at the table, etc., etc. I have learned to let go of my reaction of fear and distress, to stop and wait patiently, because then slowly the information comes back. At this point it is a matter of a lag time rather than an absolute memory loss, but I do not trust that it won’t become an absolute loss.
I am currently bothered by my memory and processing deficits, or slowness, in a book group. This is a group of highly intelligent women with very interesting things to say, but some naturally speak quickly, and there is a lot of information. It can be hard for me to follow, even impossible with fast talking, and even with the slower speakers, I find I have forgotten most of what was said afterwards. IF I were only speaking with one person, a good friend, I could request slower speech, but with a group, I feel it would be too demanding to ask everyone to slow down. I am afraid I will just have to run along behind them, metaphorically, as if I were the younger sister who can’t keep up. Sooner or later, I will either face rejection or reject myself due to unfitness.
There are a hundred different examples from everyone’s life of all the ways our combined deficits or impairments downgrade our abilities to participate in our lives.
I agree that letting go of the bad feelings and judgments are necessary to wipe the slate clean, and do so again and again. But at the end of the day, these problems have indeed put me over on the sidelines.
At best I can say that from here, there is a distinctive view, and perhaps like an anthropologist and artist, I will learn to make something interesting and worthwhile of it.
So interesting that in a space of calmness or perhaps just a space of waiting – the brain has time to kind of gather itself again and shift back into automatic mode – that’s just fascinating Cecilia….
“Yes! to so much of this. If normal people only knew that !/we can forget how to drive a car, how to organize packages or objects to carry them, how to handle a fork and knife at the table, etc., etc. I have learned to let go of my reaction of fear and distress, to stop and wait patiently, because then slowly the information comes back”
I can well relate to the frustration of simply not being able to engage as effectively with people as before….that has been hard from day one; its not as bad now but it used to drive me to tears….
i just sent two instant messages on smartphone, and now am cognitively spent. this work of Dr. Lange is s important, and Im so graeful to Cort for writing about it.
i ned more time if i were to organize a good comment, as cognitive and eading, writing is the harst for me.
But i can say as a physical therapist who is also a patient often severe side of moderate now, the motor coordination problems and conversely cognitive worsening during activty, are quite distinctly noticeable to me. I wsh my physical therapists understood what was going on, but they jut ridicule me.
I usually dont contribute to these discussions, as I cant do it eloquently in a timely manner, and its too humiliating to come across half-baked as above. then if I wait til I can compose a better comment, I am behind on other things and i never get back to it or it is weeks after the discussion.
I also have symptoms worse on right side, and after very taxing exertion, my right hand and foot (not the left) shake.
Yes, I have tremors too – worse on the right, but also head and legs. Worse at times and near not there at other times. Odd! Tiredness and stress also bring this on for me.
Issie
I know, I know, many of the above deficits happen for me. I speak too soon before I’ve taken in enough of the complexities in a situation. I just blurt something out that I regret straight after. It seems impulse control is lacking. And then, many of my statements are a compression of several. I asked my doctor if he’d pay for my gym fees yesterday and only realised what I’d said when he said no. I actually meant to ask him to sign a form justifying gym and swimming activity on the grounds of health, so I could claim something back on my gym fees from my health fund. (Which he did.) Belonging to this gym is really a case of favouring hope over experience, but I keep paying anyway.
Also, I notice great deficits in attention, concentration and working memory, constantly walking away (metaphorically speaking) leaving a task unfinished. I find making a list, then verbalising the next task to myself, repeating it over and over till I do it, are all helpful tactics. When I’m shopping I’m one of those muttering older women everyone tries to avoid. I even say to myself ‘Go home, go home,’ when I’ve done everything or it all gets too much. Also motor control, balance, especially walking on uneven pavement, and involuntary movements are issues for me, as others have said above.
Thanks, Cort, for all these posts. They’re very helpful indeed.
Lynne
That lack of ‘impulse control’ really stands out for me….particularly when I first got ill…I had never heard of that before but it was a biggie…Thanks
It sounds like with the verbalizing again and again – you’re kind of pushing it into your working memory – hopefully so that it will stick.
Before I fell ill with ME I worked as a clinicial neuropsychologist for several years. I worked with all kinds of patients from young children with learning disabilities or neurodevelopment disorders, adults with traumatic brain injuries, neuropsychiatric disorders or neurological disorders, to elderly with dementia or other serious issues. Extensive testing and diagnosis of ME-patients was a part of my job.
When the patients, no matter the diagnosis, first came to us we tested them for two consecutive days, 4-6 hours every day depending on their endurance. All of my patients came back the second day and started testing as they did the first day. But the ME-patients came back pale, trembling and with an endurance of near zero. This surprised me and my colleagues to such an extent that we changed the testing-regime for ME-patients, simply postponing day two of testing by several weeks to make them recover.
And it «worked» – with two-day testing separated by weeks the ME-patients didn’t exhibit that much cognitive deficit and problems. I wonder what would have happened to the test-result had we continued the two-consecutive-day testing? I bet we would have uncovered cognitive deficits to a much larger extent. But we simply couldn’t push them trough it, it would have been immoral («First, do not harm»), they were too sick day two.
The irony of it all is that I fell ill with the same disease myself a couple of years later. Early on in my training and work as a clinical neuropsychologist I had no doubt that myalgic encephalomyelitis was a serious and real disease, but several of my colleagues didn’t accept the patients view and experience. Maybe clinicians like them have to fell ill themselves to comprehend, but it’s a shame, and clinicians like them should be ashamed.
Wow…..what a story – and to think it ended up happening to you…Thanks for sharing your experiences and your insights…
Hi Cort, I feel as if I’ve known you in some way for years as I’ve read things you’ve written for such long time. This series or these two parts on the brain/ neuro dysfunction so resonate for me. I’m grateful for all of this as .. wow, someone actually wrote what my brain ‘does’ and how hard it gets at times for me to communicate!
I think some can even go way back in time too..
(Yes; it helps a great deal to see that someone who is a Mensa has written something here!!) What a tremendous validation this is!
Currently I’m not doing especially well for a number of reasons and do worry about that stress aspect; meaning noise, being in a chaotic environment and so on. That’s where I am, where I live. I do have it down to ‘function’ outside, but I’ve a much clearer understanding of why it gets so damn difficult now.
There’s only that problem of getting others to understand. No one does save a few doctors, other patients.
All I am capable of writing. Felt I had to say something. I am posting this on G+ as I’ve done with other pieces. I do the same with almost all
ME/ CFS/ Fibro info coming my way.
Depressing but it needs to be done I feel. And I sure hope the kickstarter film takes off.
Thank you so much; more than you know.
Thanks Jane and thanks for spreading it around..Good luck!
I have sat those tests over two day and it did indeed show that I have no working memory at all.
Ouch! 🙂
Wow! It’s amazing when seemingly unrelated symptoms turn out to be part of the same problem. For example:
– when I play guitar my fingers misbehave randomly, often enough to ruin every song, even though my brain obviously remembers what to do
– walking is inexplicably tiring and painful, and dramatically helped by slowing down, using a stick, and not thinking about anything else
– when I’ve passed my acceptable activity limit, my brain becomes distant from my surroundings (to the point where I can arouse the suspicion of store detectives and airport security), and I have trouble hearing what people are saying
– simple decisions I wouldn’t normally think about are sometimes impossible to make, or I get it spectacularly wrong (eg trying to make porridge with orange juice instead of milk)
– I sometimes get angry about a change to an expected routine (eg a last minute platform alteration at the train station) till I notice how ridiculous I’m being
– after a few hours work I become stupid and unable to do my job (accounts and accounts training) or even compose an email (this post started out all over the place, but I’m getting there…… I think….:/ )
Something I find interesting is that some of these symptoms are there all the time but others kick in as my energy levels decline with activity. So for example every morning I have to focus carefully and watch what I’m doing so I don’t break things in the kitchen, yet my ability to work is the same as before I got ME, until I cross that invisible line, which at the moment is between 3.5 and 5.5 hours.
These symptoms are so weird that I didn’t realise they were happening at first — I just used to curse myself for being stupid or clumsy. It’s understandable that other people just don’t get it — like my musician friend who suggested trying a different tuning for my guitar. 🙂
Thanks for explaining this Cort! I’m looking forward to learning more about all of this as more research is completed.
Hi Rupert
I can sympathise with the guitar playing problems. Maybe we should both take up the diddley bow : )
http://en.wikipedia.org/wiki/Diddley_bow
“when I’ve passed my acceptable activity limit, my brain becomes distant from my surroundings (to the point where I can arouse the suspicion of store detectives and airport security), and I have trouble hearing what people are saying”
This really resonates with me. Normally I’m a little socially anxious particularly in crowds (who am I kidding I’m totally socially phobic!). During a crash though I can find myself slumped on the pavement in the middle of a busy town centre and completely oblivious to what’s going on around me. Its as if all mental activity has shut down just leaving what’s essential to keep me semi-conscious.
totally identify with these symptoms, but as I am reaching my limit I think I need to go and lie down now!
It’s really disconcerting when you want to say something and the words just aren’t there. My family and a few close friends are very good at interpreting my mixed up communicating and extrapolating what it is I’m trying to say. So many times I have to ask “does that make sense?” It seems to be worse for me when I’m having stimulus overload. Lately I can’t even go out with my lunch friend because trying to make a decision about what to order with background music going on and all the people, etc. just makes everything seem like a blur. Plus the PEM after because I was “out and about” makes it not worth it. I’m finding ways to adapt though, and while that’s a good thing I think it makes it harder for others to really understand just how disabling this can be. I stand there looking normal but when the receptionist asks me my phone number and i draw a blank there’s just an awkward silence for a minute till i can come up with a joke about never calling myself. Then I feel stupid and under pressure but how do you tell someone it’s too much pressure to give your phone number? When I get to the point that I’m needing to walk in slow motion I just act like I’m not in a hurry. Sit for a while and then get up and make it to the next place I can sit or lean. It’s amazing to me how articulate some of you are able to be, but I find it kind of ironic that we need to be so eloquent about how disabling this is to cognitive abilities. 🙂 It’s good for me to read about what is working for other people, even if it’s just helping a little bit. I need to feel like I am at least doing something about this. Thanks again for the encouraging and informative articles.
I have a suggestion for any of you who have given up trying to read novels due to short-term memory issues. You might want to try a Kindle, if you can afford one. The x-ray function will remember all the characters for you. Just touch x-ray at the top of the page and a list of all the characters on that page will pop up. Hit the one you can’t remember and the Kindle will take you back to all earlier references of that character. Its wonderful. Won’t help that much with plot, but for me, it allows me to enjoy reading again so I thought it might help someone else.
As for these articles, this is all so fascinating (thank you Cort!) and although I’m sorry others have the same problems with ataxia, memory, myoclonus and other neuro problems, its a comfort to know I’m not alone, since for years I seldom heard of another person with ataxia in particular. For me, it was the very first symptom of the crash that ended any kind of normal life. I believe I had battled a much milder form of the disease for years, but when my working life ended, it started with ataxia. I had just finished giving a piano lesson, stood up and couldn’t walk across the room without staggering. By the next day, muscle/joint pain was also there plus extreme weakness.
It makes me so angry whenever someone brings up deconditioning. How can a person go from being a music director, which takes a LOT of energy, to being a person having to crawl up stairs within 24 hours? And yes, I had a gazillion tests and other diseases were ruled out, although I didn’t receive a DX of CFS for about 15 years and that was about 20 years ago.
I have actually had to lie down on the sidewalk, not 20 feet from the back door because my muscles just stopped working while trying to walk the dog. After a bit of a rest, I was able to get up and drag myself into the house. I usually veer to the left, for whatever reason, but last week I found myself almost falling to my right, so I don’t know what that means, if anything. Overstimulation, such as too much noise, often affects more than my walking. I suddenly won’t be able to feed myself at a restaurant or even speak more than a slurred, garbled whisper and must be helped to a wheelchair or physically dragged along by my husband, bless his dear heart. So, more than walking can be affected, although in some other cases, I don’t really know how badly I’m being affected by noise etc. until I stand up and then see that I’m staggering like a drunken sailor once again or do something embarrassing like walk straight into a wall instead of a doorway. The wrong odor can also trigger such collapses. I was severely affected by odors years ago and am relieved that at least I’m not quite that sensitive presently. I used to have a script for an oxygen tank. If I gorked out my son or husband would hook me up until I was strong enough to go to bed and sleep it off.
Mental functions worsen considerably while I’m trying to walk to the point I sometimes find myself mumbling gibberish that doesn’t stop until I can sit down for awhile. Multiple times daily I think of something I need to do, get up, make it to the next room and promptly forget what I meant to do. Cooking is dangerous, and that’s on a GOOD day. I melted the legs off a crock pot a few years ago after foolishly leaving it on the stove and then turning on a burner and I also burned up a hot pad. Even if I read baking instructions several times, I’m lucky not to mess up anything I try to bake, no matter how careful I try to be.
These cognitive problems seem to be getting worse, which really scares me. (I’m proof-reading this now, for instance, and I think it has taken over an hour to write.) On a bad day I can seldom have a conversation with my husband without forgetting simple words, which is SO frustrating, because I used to be fairly good with words. It doesn’t happen just once, as with some normal people my age, but almost every sentence until I just give up trying to talk. Then, inexplicably, I might have a few good days or even a week when there is no ataxia, I have a little more energy and can function more normally, so I should thank my lucky stars for days like that, I guess.
Until recently I’ve been telling people how much better I am compared to the worst years with this DD because on good days I can walk through a big store with the help of a shopping cart instead of needing a scooter, but I haven’t been able to do that nearly as often this past year and the other neuro problems are worse, so its a real roller coaster ride, as it is for everyone, I’m sure. I no longer consider myself improving, which is a real bummer and I’ve been struggling a lot to keep from becoming very depressed. Well boo hoo…geez – sorry. I know I’m a lot better off than those who are stuck in bed.
Good luck to all of you who are trying various methods to help with the cognitive problems or racing thoughts or anxiety. I’m glad meditation helps but I prefer listening to music. To me, that’s as good as any form of meditation.